by Elizabeth E. Hogue, Esq. | Sep 27, 2024 | Admin, Advocacy, Audits, Regulatory
by Elizabeth E. Hogue, Esq.
The "Wicked Witch" Chevron is Gone
On June 28, 2024, the U.S. Supreme Court overturned a decision of the Court in 1984 often referred to as “Chevron.” The Chevron case said that Courts must defer to administrative actions that are reasonable interpretations of ambiguous statutory language.
In Loper Bright Enterprises v. Raimondo, however, the U.S. Supreme Court abandoned the decision in Chevron and said that:
-
- The “deference that Chevron requires of courts reviewing agency action cannot be squared with” the Administrative Procedure Act (APA). The APA “specified that courts, not agencies, will decide ‘all relevant questions of law’ arising on review of agency action…even those involving ambiguous laws – and set aside any such action inconsistent with the law as they interpret it.”
- The framers of the U.S. Constitution envisioned that the final “interpretation of the laws” would be “the proper and peculiar province of the courts.”
- The views of the executive branch should inform the judgment of the judiciary, not supersede it.
- “Chevron’s presumption is misguided because agencies have no special competence in resolving statutory ambiguities. Courts do.”
What Does it Mean for Providers?
The short answer is that we don’t know yet. It is unclear how the new standards of the Loper Bright decision will be applied and affect health care providers. The Supreme Court said that the recent Court decision does not call past cases into question that were based on Chevron, but existing regulations are not insulated from challenges. It is likely that several providers will “swing for the fences” for favorable rulings based on Loper Bright!
One possible “candidate” for disruption is the reliance of administrative law judges (ALJs) on Chapter 8 of the Medicare Program Integrity Manual. This section offers an overview of use of inferential statistics and statistical sampling to estimate overpayments in Medicare audits. Chapter 8 of the Manual is only nine pages long. ALJs routinely use this section of the Manual to hamper providers’ ability to mount a compelling defense that challenges auditors’ methods using widely accepted standards within the statistical community. Challenges to this practice based on Loper Bright may prevent ALJs from reliance on these sections of the Manual.
Another possible target is the use of sub-statutory and even sub-regulatory guidance from the Centers for Medicare and Medicaid Services (CMS) and the Medicare Administrative Contractors (MACs) by fraud and abuse enforcers to make determinations about illegal conduct, especially under the False Claims Act (FCA). Defendants arguably now have a better chance to challenge the basis of claims of illegal conduct in light of Loper Bright.
The story of Loper Bright has not been written by any means. Surely providers should use this significant change in the law to their benefit whenever possible.
Elizabeth Hogue is an attorney in private practice with extensive experience in health care. She represents clients across the U.S., including professional associations, managed care providers, hospitals, long-term care facilities, home health agencies, durable medical equipment companies, and hospices.
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
©2024 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
by Elizabeth E. Hogue, Esq. | Aug 9, 2024 | Admin, Clinical, Regulatory
by Elizabeth E. Hogue, Esq.
HIPAA violation: Trent James Russell was convicted in federal Court on charges of obtaining another person’s health care information in violation of the Health Insurance Portability and Accountability Act (HIPAA). Russell was employed by an organ transplant organization. As a transplant coordinator, he had access to electronic medical records at George Washington University Hospital in Washington, DC.
In January of 2019, Russell accessed the medical records of U.S. Supreme Court Justice Ruth Bader Ginsburg even though Justice Ginsburg had not been referred as a possible organ donor. He took a screenshot of the records and then posted them on a message board called “4chan.” Ginsberg’s records quickly appeared on Twitter and YouTube, including her name and the exact dates and times when she received radiology, oncology, and surgical treatments at the Hospital between 2014 and 2018.
Hospital officials traced the search of Ginsburg’s records to one of Russell’s home computers. As soon as Russell was identified as a suspect, his access was denied by the Hospital. His request to have access restored was also denied.
The Cat Made me Violate HIPAA Laws
Russell initially told federal agents that his “cats had run across his keyboard.” He later characterized this statement as a “nervous joke.” Russell said that he had no idea how his computer searched terms that produced the Justice’s records and that “everyone makes typos.”
Online users who viewed Ginsberg’s records promoted various antisemitic conspiracy theories. One theory was that Ginsburg had died in late 2018 and that democrats were hiding her death in order to deny President Trump an opportunity to appoint her replacement. A search of Russell’s computer also revealed a search for the term “dirty jew.”
An FBI agent said that she found an image on Russell’s hard drive that mimicked a poster for the film “Weekend at Bernie’s.” The caption said “Weekend at Ginsburg’s” and showed leaders of the U.S. House of Representatives propping Ginsburg up from both sides in a morbid play on how the movie characters covered up Bernie’s death so that they could use his beach house.
Ignorance of HIPAA Law is not a Defense
But, he didn’t even have that. The Chief Executive Officer of the transplant organization at the time the access occurred testified that coordinators like Russell had “no business being inside the chart” of patients who had not been referred to the organization. The CEO said that Russell was certainly aware of this prohibition because of numerous agreements he signed with his employer and the extensive training he received.
There are several important takeaways from this case. First, it is important to note that Russell had extensive training about the requirements of the HIPAA Privacy Rule. He also agreed to comply with these requirements. The temptation is great, but employees must be reminded not to succumb. In addition, practitioners should take note of the fact that Russell was criminally prosecuted. Since he was convicted, he faces up to twenty-two years in prison and fines in the tens of thousands of dollars. Serious business!
Elizabeth Hogue is an attorney in private practice with extensive experience in health care. She represents clients across the U.S., including professional associations, managed care providers, hospitals, long-term care facilities, home health agencies, durable medical equipment companies, and hospices.
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
©2024 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
by Elizabeth E. Hogue, Esq. | Aug 1, 2024 | Clinical
by Elizabeth E. Hogue, Esq.
What do Managed Care Plans Really Want from Providers of Services to Patients in Their Homes?
Medicare Managed Care Plans have a long history of disinterest in provision of services to patients in their homes. Despite the fact that they are mandated to provide the same services that enrollees in Medicare fee-for-services receive, they just haven’t done it. Common practices among Plans of draconian, untimely preauthorization processes and doling out authorizations for visits a few at a time make it clear that Plans have seen no real value in services to patients at home.
Plans, of course, should have been very interested in services at home. These services save money and keep patients at home where they want to be. Services at home are just generally a beautiful thing!
At the same time, it’s fair to say that the Office of Inspector General (OIG) of the U.S. Department of Health and Human Services (HHS), the primary enforcer of fraud and abuse prohibitions, has Medicare Managed Care Plans in its crosshairs. A key area of concern for the OIG is that Medicare Managed Care Plans make visits to patients in their homes looking for additional diagnoses so that the Plans will receive more money per patient. The OIG is especially critical of this practice because review of medical records of patients who received visits at homes and whose acuity increased as a result never received any care for these new diagnoses.
Managed Care Plans in the News
The Wall Street Journal recently reported that between 2018 and 2021 Plans received $50 billion for diagnoses added to members’ charts, at least some of which resulted from visits to patients in their homes.
After years of disinterest, Plans are now quite interested in at home services. Is it possible that Plans’ newfound interest is related to a desire to increase revenue through home visits? It appears so. Take, for example, comments by the CEO of UnitedHealth Group, Andrew Witty, during an investment call on July 16, 2024.
Managed Care Plan Responds

UnitedHealth Group CEO Andrew Witty
Mr. Witty reported to investors that staff made more than 2.5 million home health visits to Plan members in 2023. “As a direct result, our clinicians identified 300,000 seniors with emergent health needs that may have otherwise gone undiagnosed,” Mr. Witty said. “They connected more than 500,000 seniors to essential resources to help them with unaddressed needs.”
Former UnitedHealth employees told The Wall Street Journal that home visits were used to add diagnoses to patients’ records. They said that clinicians used software during visits that offered suggestions about what illnesses patients might have.
It now looks like it’s possible that at-home care is being hijacked by Medicare Advantage Plans to help Plans engage in practices that the OIG views as questionable.
Elizabeth Hogue is an attorney in private practice with extensive experience in health care. She represents clients across the U.S., including professional associations, managed care providers, hospitals, long-term care facilities, home health agencies, durable medical equipment companies, and hospices.
©2024 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
by Elizabeth E. Hogue, Esq. | Jul 26, 2024 | Regulatory
by Elizabeth E. Hogue, Esq.
Dept of Health & Human Services Final Rule
On May 7, 2024, the U.S. Department of Health and Human Services (HHS) issued a final rule establishing the first federal regulations for Adult Protective Services (APS). The regulations took effect on June 7, 2024. The entire rule is at https://acl.gov/apsrule.
One goal of the new regulations is to promote high quality APS that better meet the needs of adults who experience or are at risk of maltreatment and self-neglect. Another goal is to improve consistency in services among the states.
APS services have historically been funded by state and local governments. There has been wide variation in APS services and practices between and even within states. New regulations, along with recent funding from HHS to state APS programs, now make it possible to improve consistency.
-
- Establishes a set of national minimum standards for the operation of APS programs that all state APS systems meet
- Requires APS systems to ensure that planning and delivery of all services respect the fundamental right of adults to make their own life choices and that services are driven by the person receiving them
- Establishes stronger protections for clients subject to, or at risk of, guardianship. Specifically, APS must consider guardianship only when there are not alternatives.
- Requires responses within 24 hours of screening cases that are life-threatening or likely to cause irreparable harm or significant loss of income, assets, or resources
- Requires APS to provide at least two ways, at least one of which must be online, to report maltreatment or self-neglect 24 hours per day, seven days per week
- Requires robust conflict of interest policies to support ethical APS practice
- Establishes definitions for key APS terms to improve information sharing, data collection, and program standardization
- Promotes coordination and collaboration with state Medicaid agencies, long-term care ombudsmen, tribal APS, law enforcement, and other partners.
The Need for Adult Protective Services
HHS points out that at least one in ten older adults who live in communities experience some form of maltreatment each year.
All providers have been involved in situations in which adult protective services are needed. Case managers/discharge planners in hospitals and long-term care facilities are especially likely to encounter and to be expected to assist with situations involving APS.
Providers of services to patients in their homes; including home health agencies, hospices, home medical equipment (HME) companies, and home care or private duty companies; are on the “front lines” with regard to identifying situations in which APS is needed. At least anecdotally, however, providers have received very little assistance and support from APS in situations of abuse and neglect.
Hopefully, providers can look forward to greater assistance in view of enhanced funding and standards.
Elizabeth Hogue is an attorney in private practice with extensive experience in health care. She represents clients across the U.S., including professional associations, managed care providers, hospitals, long-term care facilities, home health agencies, durable medical equipment companies, and hospices.
©2024 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
by Elizabeth E. Hogue, Esq. | Jul 19, 2024 | Admin, Regulatory
by Elizabeth E Hogue, Esq.
Three home health agencies and their parent company in Cincinnati, Ohio, must pay $4,496,330 to resolve alleged violations of the federal False Claims Act by providing kickbacks to assisted living facilities in exchange for referrals of Medicare patients. The settlement resolves allegations that, between 2013 and 2022, the companies provided lease payments and other valuable benefits; including wellness health services, sports tickets, and meals; to numerous ALFs and their residents. The companies then billed Medicare for the services provided to patients referred by the ALFs.
Getting more referrals from ALF’s and retirement communities seems to be a crucial piece of the puzzle for all types of providers. As the number of years in which they have been in business increases, ALF’s and retirement communities are more eager to assist their residents to “age in place.” This means that they often view availability of services from post-acute providers as essential to allow them to achieve this goal.
While providers compete aggressively in the marketplace, they cannot, however, lose sight of the fact that the healthcare industry is highly regulated. With ever-increasing emphasis on fraud and abuse compliance, providers cannot afford to violate the law.
How can providers get more referrals from ALF’S and retirement communities? What are the potential legal pitfalls that providers must avoid?
The most effective way to maximize referrals from these sources may be to take a multi-pronged approach that includes:
Assigning at least one coordinator/liaison to each referral source on at least a part-time basis
Use of coordinators/liaisons at ALF’s and retirement communities raises issues related to violation of the federal anti-kickback statute. This statute generally prohibits providers from either offering to give or actually giving anything to referral sources in order to induce referrals. Consequently, liaisons and coordinators must be scrupulous about avoiding the provision of free services to ALF’s and retirement communities and/or their residents. Possible violations include “staffing” an office with an RN who responds to requests from residents in their apartments or has “office hours” to address health conditions of residents.
Renting space for coordinators/liaisons to occupy so that providers have a frequent or continuous presence on the premises of referral sources to better serve patients
Renting space from referral sources also involves potential kickbacks, so providers must meet the requirements of the space rental exception or safe harbor. In order to do so, providers must enter into a written lease with the facility/community for a term of least one year. The lease must include the number of square feet providers are renting. Rent must be set in advance at fair market value and cannot take into account either the volume or value of referrals received. Finally, providers may rent only the amount of space that is commercially reasonable or that they actually need.
The OIG has provided significant guidance about these requirements, which providers must master before they establish these types of relationships. Common pitfalls for providers is insistence by ALFs that providers must rent an entire apartment, whether or not they need it, and must pay an amount equal to the residents’ monthly rent, which includes food and other services.
Entering into Preferred Provider Agreements
Preferred Provider Agreements may be verbal or in writing. There may be significant value in reducing these preferred provider relationships to writing. These types of relationships raise issues related to patients’ right to freedom of choice of providers. The common law or court decisions require providers of all types to honor patients’ right to freedom of choice. There are also federal statutes that guarantee this right to Medicare and Medicaid patients. In addition, states sometimes address these issues in applicable statutes and regulations. For this reason, providers should not attempt to use standard or “sample” Agreements, but must adhere to requirements in all of the states in which they use these types of Agreements.
Providing a full range of screenings and educational events for and about common chronic illnesses or community awareness activities
ALF’s and retirement communities often ask providers to conduct educational events and basic screenings for common chronic conditions. Generally, providers may do so if they walk a relatively fine line between engaging in community awareness activities and providing free skilled services to residents that exceed $15.00 in value at a time. At a minimum, such activities must be conducted consistent with a detailed policy and procedure that governs the provision of such services, so that providers do not violate the anti-kickback statute.
Establishing relationships with ALF’s and retirement communities may result in numerous referrals to post-acute providers. Such relationships should be based on standard documents and comprehensive policies, as described above, in order to ensure compliance. Legal representation is essential for the development and implementation of these documents due to the complexity of the issues involved.
Enforcement actions like those described above are avoidable.
Elizabeth Hogue is an attorney in private practice with extensive experience in health care. She represents clients across the U.S., including professional associations, managed care providers, hospitals, long-term care facilities, home health agencies, durable medical equipment companies, and hospices.
©2024 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
by Elizabeth E. Hogue, Esq. | Jul 12, 2024 | Clinical, Privacy and Security, Regulatory
by Elizabeth E. Hogue, Esq.
Imagine that a celebrity receives care where you work and curiosity gets the better of you, or someone you know is admitted and you would love to know the details. It’s oh so very tempting! So, you access records of care provided to patients that you have no legitimate need to view. The HIPAA police are on it! Because let’s not forget that the HIPAA Privacy Rule is a criminal statute.
An emergency room physician, for example, pled guilty to illegally obtaining the personal health information of multiple individuals. He was convicted of one count of wrongfully obtaining individually identifiable health information under false pretenses. The physician received a resident physician license and participated in an emergency medicine residency program at a university hospital. He worked in the emergency room of two hospitals in the university system.
The doctor used his access as a resident physician to the hospitals’ electronic health record to access the records of two patients without their knowledge or consent. He was never the patients’ physician. The patients were not receiving care in the emergency rooms where the doctor worked at the time he accessed the records.
The doctor also admitted that he sent a photograph to someone else of one of the patients wearing a hospital gown in which the patient’s rectum was hanging out of the patient’s body. And now for the “best” part: the doctor also admitted that he falsely wrote in a letter that he sent the picture of the patient with a prolapsed rectum to his mother to remind her of the importance of fiber intake!
Do you remember the comedian, Flip Wilson, who repeatedly claimed that the devil made him do it? When it comes to accessing patients’ medical records in violation of HIPAA, you must “put the devil behind you!” Protecting patients’ private health information is serious business – serious criminal business. Be vigilant!
By the same token, providers must also always remember that the HIPAA Privacy Rule isn’t just about protecting health information; it’s also about giving appropriate access to it. In the zeal to protect information, it anecdotally seems that practitioners have lost sight of the fact that access to information is at least as important as protection of information. In fact, the Office for Civil Rights, the federal enforcer of HIPAA violations, has focused on denial of access in enforcement actions for the past several years.
Remember that, however tempting the information you would like to have may be, temptation pales in comparison to jail time!
Elizabeth Hogue is an attorney in private practice with extensive experience in health care. She represents clients across the U.S., including professional associations, managed care providers, hospitals, long-term care facilities, home health agencies, durable medical equipment companies, and hospices.
©2024 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
by Elizabeth E. Hogue, Esq. | Jun 20, 2024 | Admin, Caring for the Caregiver, Clinical, CMS
By Elizabeth E. Hogue, Esq.
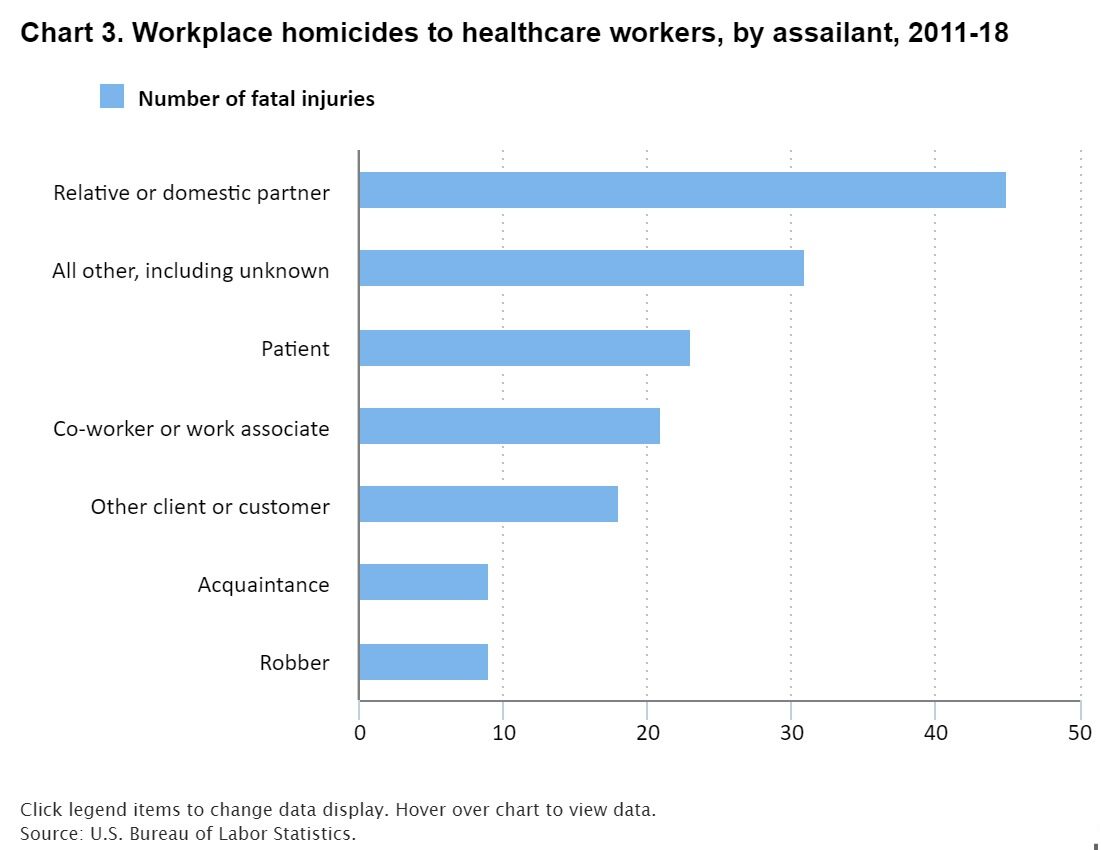
Violence in Healthcare
According to a recent analysis of Bureau of Labor Statistics data, healthcare is one of the most dangerous places to work. Homecare field staff members who provide services on behalf of private duty agencies, hospices, Medicare-certified home health agencies, and home medical equipment (HME) companies may be especially vulnerable. Contributing to their vulnerability is the fact that they work alone on territory that may be unfamiliar and over which they have little control. Staff members certainly need as much protection as possible.
Must-Haves
First, regardless of practice setting, management should develop a written policy of zero tolerance for all incidents of violence, regardless of source. The policy should include animals. The policy must require employees and contractors to report and document all incidents of threatened or actual violence, no matter how minor. Emphasis should be placed on both reporting and documenting. Employees must provide as much detail as possible. The policy should also include zero tolerance for visible weapons. Caregivers must be required to report the presence of visible weapons.
Below are some additional important actions for healthcare organizations to take that are based on UCHealth’s SAFE Program:
- Encourage staff members to STOP if they feel unsafe for any reason.
- Workers should pause to generally ASSESS their environments. Staff members should think about what has happened and observe what is currently occurring. Is there, for example, mounting frustration or anger?
- Staff should then FAMILIARIZE themselves with the room. Who is the patient? Where is the patient? Are there any factors that might escalate behaviors? Staff members should also consider putting themselves in positions where they have a route to escape, if necessary.
- Practitioners should also ENLIST help. Getting help may, for example, include pushing panic buttons on mobile devices.
Here is what Chris Powell, Chief of Security at UCHealth said in Becker’s Hospital Review on June 4, 2024:
“You can’t just talk about the shrimp and give you a good picture. We have to talk about the roux and the rice and everything else that goes into this for a good picture to be painted so people have an understanding. We want to solve this with an electronic learning or a 15-minute huddle, but we can’t. This is continuous and a persistent pursuit toward educating, communicating, recognizing, responding to, reporting and recovering from workplace violence.”
Every caregiver matters. The healthcare industry has lost caregivers to violence on the job in the past. Let’s not repeat these terrible events.
©2024 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
by Elizabeth E. Hogue, Esq. | May 30, 2024 | Admin, Regulatory
by Elizabeth E. Hogue, Esq.
The National Labor Relations Board (NLRB) has now joined the Federal Trade Commission (FTC) and some state legislatures to target non-compete agreements. The general counsel for the NLRB argued in a recent memo that non-compete agreements violate the National Labor Relations Act because they interfere with employees’ right to engage in protected concerted activity. Two recent actions by the Board provide more information about efforts of the NLRB to limit use of non-compete agreements.
Juvly Aesthetics Non-Compete Agreement Settlement
In February of 2024, the regional office of the Board in Cincinnati approved a settlement agreement between Juvly Aesthetics and three former employees. The Board claimed that Juvly, an operator of medical clinics, violated the rights of employees through the use of confidentiality, non-disparagement, non-competition, non-solicitation and requirements to repay training expenses under certain conditions.
According to the NLRB, Juvly prohibited employees from discussing their rates of pay. The Company also required some employees to sign a non-compete agreement that was in effect for a period of twenty-four months for any competing medical practice within twenty miles of any location of the Company.
Juvly agreed to a settlement agreement that required:
- Payment of back pay to some employees
- Termination of unlawful policies and procedures
- Release of employees from unlawful agreements
- Posting of all of requirements of the settlement agreements for review by employees
In December, the NLRB Division of Advice issued guidance that evaluated the legality of these issues:
- Customer non-solicitation provisions do not violate the Act because they only prevent employees from soliciting existing customers for one year so that employees are likely not barred from other employment opportunities for more than one year.
- Confidentiality agreements do not violate the Act because they prohibit only disclosure of trade secrets, marketing plans, customer lists, and other proprietary information, as opposed to information that could involve employee activity regulated by the Act, such as wage information.
- Provisions requiring the return of company property do not violate the Act.
Providers are now clearly operating in an environment that prohibits employers from restricting employee activities that were fair game in the past. The specifics of efforts to limit the actions of employers remain unclear, but will likely be “fleshed out” in enforcement actions.
©2024 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
by Elizabeth E. Hogue, Esq. | May 2, 2024 | Clinical
by Elizabeth E. Hogue, Esq.
Noora Health has developed a program of “health companions” in a variety of types of healthcare settings (“Teaching Patients How to Heal,” The New York Times, April 14, 2024) to help patient heal. The basis of these programs is that when medical information is properly communicated to patients and their families, complications of surgeries and illnesses are reduced. An added bonus is that acts of violence by frustrated family members against health care workers are reduced.
If patients are most comforted by their loved ones, why not involve them in the healthcare process? “We realized that caregivers get little to no guidance within the health care system,” said Shahed Alam, a co-founder of Noora Health. Many patients do not know why they are receiving care. Doctors and nurses tend repeat the same information to patient after patient.
“We realized that caregivers get little to no guidance within the health care system,” said Shahed Alam, a co-founder of Noora Health. Many patients do not know why they are receiving care. Doctors and nurses tend repeat the same information to patient after patient.
In institutional settings, staff nurses literally take over the floors to teach patients and their family members. On cardiac floors, for example, staff nurses tell patients how to cough without stressing their hearts, how to scratch without adversely affecting their wounds, and how pacemakers work. Staff nurses also help patients sift through good and bad information. Classes frequently include how to manage side effects of medications and the importance of handwashing.
Many patients and their family members come to view the staff nurses as therapists, coaches, friends and philosophers all rolled into one. A family member who received help from a health companion described the companion as a “friend” without whom she would not have been able to care for her family member.
Although home care providers, including Medicare certified home health agencies, hospices, private duty home care agencies, and durable medical equipment (DME) companies do not necessarily have a “captive audience” like institutional providers, it is still possible to utilize health companions. Field staff can be trained to provide teaching that is similar to that provided by health companions. Teaching from health companions may also be provided to home care patients and their family members in group settings. Hospices may, for example, provide volunteers to be with patients while their caregivers attend. And, of course, virtual teachings with health companions may also prove valuable.
Providers often consider ways to differentiate their services in a competitive marketplace. Perhaps the use of health companions is one way to do so, Providers may also enhance loyalty from patients and their families, improve quality of care and prevent emergency room visits, hospitalizations and rehospitalizations. Think about it!
©2024 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
©2024 This article appeared in The Rowan Report. All rights reserved.
by Elizabeth E. Hogue, Esq. | Apr 18, 2024 | Clinical, Regulatory
by Elizabeth E. Hogue, Esq.
Some owners and managers of private duty home care agencies mistakenly think that fraud and abuse prohibitions apply only to services paid for by the Medicare Program. In fact, fraud and abuse prohibitions apply to providers if they accept any state or federal funds, including, but not limited to, Medicaid, Medicaid waiver, VA, and Tri-Care. Many private insurers have adopted the prohibitions on fraud implemented by state and federal programs.
Private duty home care agencies are increasingly in the crosshairs of fraud enforcers if they receive reimbursement from Medicaid and/or Medicaid Waiver Programs. The reason for enhanced scrutiny is that both the federal government, which partially funds state Medicaid and Medicaid Waiver Programs, and state governments that also fund these programs are alarmed about the high costs of them.
Conventional wisdom says that there are big bucks to be saved if fraud and abuse in the Programs are controlled and ultimately eliminated. Conventional wisdom also says that enforcement actions in Medicaid Programs have just scratched the surface. According to this “wisdom,” there are big bucks to be recouped from “low-hanging fruit!”
A recent report from the Office of Inspector General of the U.S. Department of Health and Human Services seems to support this perception regarding private duty home care agencies based on the following:
 Between 2014 and 2023, at least 34% of fraud convictions in some years were based on private duty home care services. In some years, this percentage was as high as 48%.
Between 2014 and 2023, at least 34% of fraud convictions in some years were based on private duty home care services. In some years, this percentage was as high as 48%.- In fiscal year 2023, there were 279 criminal convictions related to private duty home care services compared to 66 for registered nurses and 43 for home health agencies.
- Recoveries from private duty home care agencies in 2023 totaled $26.4 million.
- The amount of civil recoveries reached a 4-year high in 2023 and the combined criminal and civil recoveries were $1.2 billion, resulting in a return on investment of $3.35 for every $1 spent.
The return on investment of more than three times the amount spent is perhaps the most important figure of all. With a three to one return, regulators will not hesitate to “beef up” enforcement actions.
THE CONSEQUENCES OF FRAUD AND ABUSE ARE SEVERE WHEN SERVICES ARE PAID FOR BY THE MEDICAID AND OTHER STATE AND FEDERAL PROGRAMS!
Personal care private duty agencies, don’t believe the myth that only services paid for by the Medicare Program are subject to fraud and abuse enforcement. The consequences may be devastating, including the loss of businesses. Heads up!
©2024 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
©2024 This article appeared in The Rowan Report. All rights reserved.












 “We realized that caregivers get little to no guidance within the health care system,” said Shahed Alam, a co-founder of Noora Health. Many patients do not know why they are receiving care. Doctors and nurses tend repeat the same information to patient after patient.
“We realized that caregivers get little to no guidance within the health care system,” said Shahed Alam, a co-founder of Noora Health. Many patients do not know why they are receiving care. Doctors and nurses tend repeat the same information to patient after patient. Between 2014 and 2023, at least 34% of fraud convictions in some years were based on private duty home care services. In some years, this percentage was as high as 48%.
Between 2014 and 2023, at least 34% of fraud convictions in some years were based on private duty home care services. In some years, this percentage was as high as 48%.

