AI in Home Care
by Laurie Orlov, Founder, Aging and Health Technology Watch
The Future of AI in Home Care
New Research Report
Wed, 06/04/2025
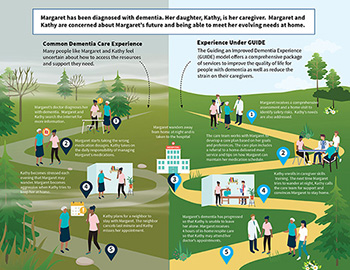
PORT SAINT LUCIE, FL, UNITED STATES, June 4, 2025 /EINPresswire.com/ — The home care industry is facing a crisis. Driven by demographic shifts, longer life expectancy, and rising rates of chronic illness and cognitive decline, the demand for in-home personal care and home health care is surging. This will accelerate as the baby boomers age into their later years – in January, the oldest of the 76 million baby boomers will turn 80. At the same time, the care industries will face a critical shortage of all categories of care delivery, with millions of additional workers needed over the next decade. Against this backdrop, AI technology has emerged to help older adults in multiple ways. In a 2023 report, The Future of AI and Older Adults, AI was already able to produce insights about a person’s health needs and offer a chatbot to help with post-hospital care. In a subsequent 2023 report, AI and the Future of Care Work, it was apparent that AI could help generate an appropriate care plan and that an ‘AI Caregiver’ role was emerging to supplement in-person care delivery. In the 2024 report, The Future of AI in Senior Living and Care, AI was being used to analyze hospital discharge information to compare patient needs to nursing home capacity.
Today there are many more initiatives and new possibilities for addressing multiple aspects of both private duty home care and home health operations, including assistance with recruiting and onboarding workers, using data to create and update care-related documents, and introducing AI agents that can be assigned to complete specific tasks. As current industry leaders note, AI tech is playing a role in care oversight and enabling the creating of hybrid models – an increasingly likely combination of in-person care supplemented with AI.

This report draws insights from experts across home care, home health care, plus software and device providers, and healthcare sectors to examine how AI is currently being used and suggest what lies ahead within the next five years.
The report can be found at this link: https://www.ageinplacetech.com/page/future-ai-home-care
# # #


Laurie M. Orlov, a tech industry veteran, writer, speaker, elder care advocate, is the founder of Aging and Health Technology Watch — market research, trends, blogs and reports that provide thought leadership, analysis and guidance about health and aging-related technologies and services that enable boomers and seniors to sustain and improve their quality of life. In her previous career, Laurie spent many years in the technology industry, including 9 years at analyst firm Forrester Research. She has spoken regularly and delivered keynote speeches at forums, industry consortia, conferences, and symposia, most recently on the business of technology for boomers and seniors. She advises large organizations as well as non-profits and entrepreneurs about trends and opportunities in the age-related technology market. Her perspectives have been quoted in the Wall Street Journal, the New York Times, Vox, Senior Housing News, CNN Health, AARP Bulletin and Consumer Reports. She has a graduate certification in Geriatric Care Management from the University of Florida and a BA in Music from the University of Rochester. Laurie has provided testimony about technology at a Senate Aging Committee hearing and has consulted to AARP. Advisory clients have included AARP, AOL, Argentum, Bose, Calix, CDW, Microsoft, Novartis, and Philips. Her reports include: The Market Overview Technology for Aging 2025, The Future of AI in Senior Living and Care, The User Experience Needs An Upgrade 2024, The Future of AI and Older and Older Adults 2023, The Future of Care Work and Older Adults 2023, The Future of Sensors and Older Adults 2022, Beyond DIY: The Future of Smart Homes and Older Adults 2021, and The Future of Wearables and Older Adults 2021. Laurie has been named one of the Women Leaders in Voice, Top 50 Influencers in Aging by Next Avenue and one of the Women leading global innovation on AgeTech.
©2025 by Aging and Health Technology Watch. All rights reserved. This introduction and link are printed with permission from the author. For more information or to request usage rights, please contact Laurie Orlov.