Chief Government Affairs Officer Announced
FOR IMMEDIATE RELEASE
Contacts: Elyssa Katz
571-281-0220
Thomas Threlkeld
202-547-7424
communications@allianceforcareathome.org
The National Alliance for Care at Home Welcomes Scott Levy as Chief Government Affairs Officer
WASHINGTON, D.C., JAN 21, 2025. The National Alliance for Care at Home (the Alliance) is excited to announce Scott Levy as its inaugural Chief Government Affairs Officer starting on January 27. With over 20 years of distinguished experience in government relations, public policy, advocacy, and law, Scott is poised to lead the Alliance’s efforts to drive impactful legislative and regulatory changes that expand access to quality care at home for America’s growing population of elderly and seriously ill.
“Scott Levy is an extraordinary addition to our leadership team. He brings a deep understanding of healthcare policy, politics, and a great sensitivity to the intersection of public policy and healthcare operations and how policy impacts patients and families. His track record of success, combined with his dedication to improving care at home, makes him an invaluable addition to our team.”
Background and Experience
Scott’s career is marked by notable achievements and experiences in both the public and private sectors. He most recently served as Chief Government Affairs Officer at Amedisys, one of the nation’s largest at-home healthcare providers, where he led initiatives that secured critical legislative and regulatory reforms, including payment model adjustments and the expansion of value-based care. His public service includes roles with all branches of government at both the state and federal level, where he gained invaluable experience in high-level government operations and policymaking.
His skill set as a lawyer, where he has advocated for clients in regulatory settings and in the courtroom, combined with his political experience and decade of service to one of the largest providers in our industry make Scott uniquely qualified for this role at this time.
Education
A graduate of Louisiana State University, Scott earned both a Bachelor of Arts in Political Science and a Bachelor of Arts in Mass Communication before completing his Juris Doctor at the LSU Paul M. Hebert Law Center. His legal and policy expertise, as well as his strategic leadership, has made him a trusted advisor to CEOs, boards, and industry leaders across the healthcare landscape.
Chief Government Affairs Officer Role
At the Alliance, Scott will lead a talented team of advocacy professionals and work closely with policymakers, industry stakeholders, and grassroots networks to address challenges such as provider reimbursement, regulatory hurdles, improving quality and program integrity, and advancing innovative care models. His leadership will strengthen the Alliance’s ability to represent and empower its members while ensuring better access to home-based care for patients and their loved ones nationwide.
In His Own Words
“I am honored and humbled to join the inaugural executive leadership of the Alliance. This opportunity allows me to leverage and maximize my nearly ten years of experience in advocating for home health and hospice on the state and national level. I am eager to get started in strategically positioning the industry and aggressively pursuing public policy that ensures all Americans can access quality care in the home. I look forward to working with and leading a unified care at home community as we make our positions known and voices heard in Washington.”
We are honored to welcome Scott Levy to the Alliance and look forward to the transformative impact of his leadership!
# # #
About the National Alliance for Care at Home
The National Alliance for Care at Home (the Alliance) is a new national organization representing providers of home care, home health, hospice, palliative care, and other health care services mainly delivered in the home. The Alliance brings together two organizations with nearly 90 years of combined experience: NAHC and NHPCO. NAHC and NHPCO have combined operations to better serve members and lead into the future of care offered in the home. Learn more at www.AllianceForCareAtHome.org.
©2025 National Alliance for Care at Home. This press release originally appeared on The Alliance website and is reprinted on The Rowan Report with permission.


 Right at Home will provide in-home care and safety assessments for eligible beneficiaries to evaluate the safety of the home environment, to assess the ability of the beneficiary to manage and function at home, and to report to PocketRN other environmental, social, and behavioral factors that might impact the function and needs of the beneficiary and their caregiver. PocketRN and Right at Home will use these valuable reports to bring other resources included in the GUIDE benefit package to better support the beneficiary and allow them to stay in their home longer.
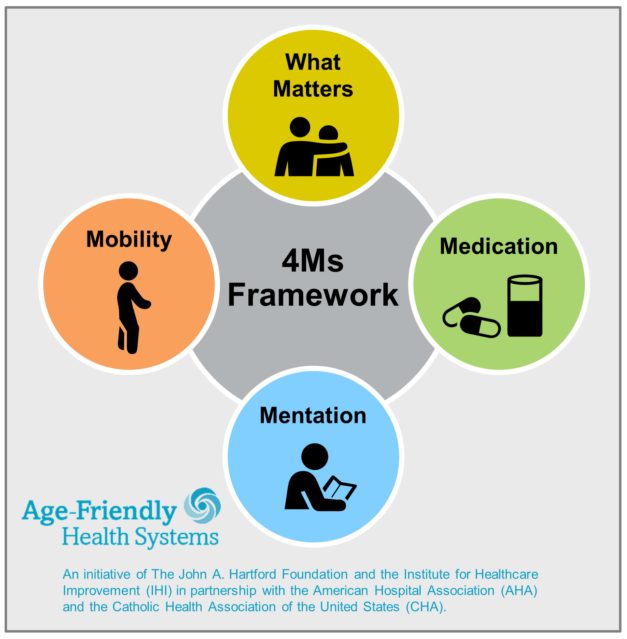
Right at Home will provide in-home care and safety assessments for eligible beneficiaries to evaluate the safety of the home environment, to assess the ability of the beneficiary to manage and function at home, and to report to PocketRN other environmental, social, and behavioral factors that might impact the function and needs of the beneficiary and their caregiver. PocketRN and Right at Home will use these valuable reports to bring other resources included in the GUIDE benefit package to better support the beneficiary and allow them to stay in their home longer. The CMS GUIDE Model, launched on July 1, 2024, introduces a new payment framework to ensure that individuals living with dementia receive holistic, person-centered care. It tackles caregiver burnout by offering respite care services to allow caregivers necessary breaks to maintain their health and well-being. The program also improves access to care by providing 24/7 availability of trained professionals through telehealth services, overcoming geographic barriers and ensuring equitable support. Additionally, it addresses training deficits with Nevvon’s multilingual, on-demand e-training modules, which empower caregivers with the skills and knowledge to navigate the complexities of dementia care. PocketRN’s “virtual nurse for life” model bridges fragmented services by connecting caregivers, patients, and clinicians, creating a seamless, coordinated care experience.
The CMS GUIDE Model, launched on July 1, 2024, introduces a new payment framework to ensure that individuals living with dementia receive holistic, person-centered care. It tackles caregiver burnout by offering respite care services to allow caregivers necessary breaks to maintain their health and well-being. The program also improves access to care by providing 24/7 availability of trained professionals through telehealth services, overcoming geographic barriers and ensuring equitable support. Additionally, it addresses training deficits with Nevvon’s multilingual, on-demand e-training modules, which empower caregivers with the skills and knowledge to navigate the complexities of dementia care. PocketRN’s “virtual nurse for life” model bridges fragmented services by connecting caregivers, patients, and clinicians, creating a seamless, coordinated care experience.



 Launched on July 1, 2024, the GUIDE Model will test a new payment approach for key supportive services furnished to people living with dementia, including: comprehensive, person-centered assessments and care plans; care coordination; 24/7 access to an interdisciplinary care team member or help line; and certain respite services to support caregivers. People with dementia and their caregivers will have the assistance and support of a Care Navigator to help them access clinical and non-clinical services such as meals and transportation through community-based organizations.
Launched on July 1, 2024, the GUIDE Model will test a new payment approach for key supportive services furnished to people living with dementia, including: comprehensive, person-centered assessments and care plans; care coordination; 24/7 access to an interdisciplinary care team member or help line; and certain respite services to support caregivers. People with dementia and their caregivers will have the assistance and support of a Care Navigator to help them access clinical and non-clinical services such as meals and transportation through community-based organizations.