OASIS, OASIS Everywhere!
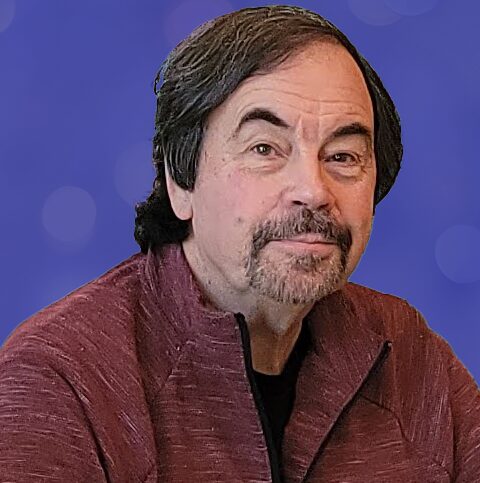
by Tim Rowan, Editor Emeritus
OASIS, OASIS, Everywhere
At this year’s annual meeting of The National Alliance for Care at Home, one could not attend a general or breakout session or walk an aisle in the exhibit hall without hearing about artificial intelligence. After 27 years covering Home Health, Home Care, and Hospice technology, I have seen buzzwords come and go. Declared game-changers have evolved from Windows to the iPad, to smartphones, to telehealth, to Big Data, to the Internet itself.
Interestingly enough, the “game” never changed. Patients/clients, nurses/CNAs, claims, payroll, and A/R have always, and will always, keep owners, administrators, and managers sprinting. AI will bring massive changes, but not to these constants.
AI is a Supplement, not a Replacement
There is much concern, and a plethora of articles, about how easily AI can be abused, even with the most noble intentions. We have detected serious concern about a movement to allow AI to make clinical decisions. We concur that this is inappropriate. Advising clinical decisions, providing background on previous patients with similar symptoms, or quickly accumulating data on the history of a chronic condition, can benefit our patients and clients in ways no other technology has been able to do. Making clinical decisions is different in both kind and degree.
This is why we were impressed with the focus on supplementing over replacing that we witnessed in New Orleans.
Ambient Listening for OASIS
When WellSky acquired Kinnser, everyone wondered whether the Home Health EMR would improve or merely be maintained for its customer base. Longtime friend of The Rowan Report, and WellSky and former Fazzi consultant Cindy Campbell, RN, convinced us with her uncharacteristic effusiveness to take another look at the latest WellSky feature.

How it works
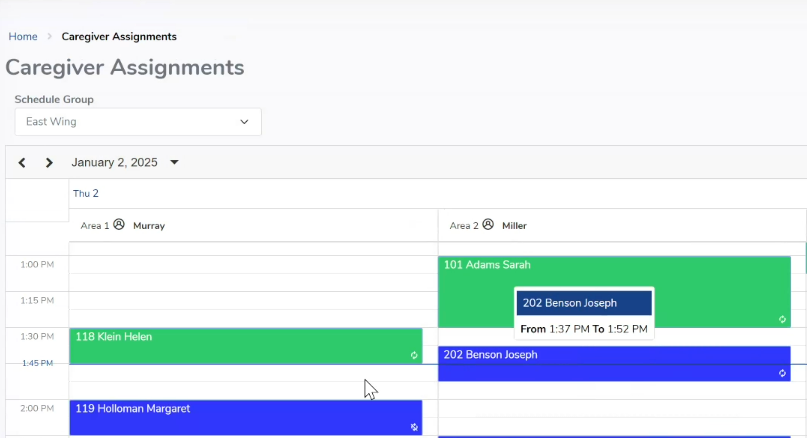
During the OASIS visit, the nurse in the home logs into an app and places it between him/her and the patient. As the normal OASIS conversation takes place, the AI-enabled app not only hears but interprets every nuance of the chat. By the time the OASIS visit is over, the agency’s EMR has been fully populated. Every OASIS question has been answered, and every numerical rating field has been accurately completed.
Human touch
Wisely, WellSky allows no AI OASIS assessment to be saved or signed without review by a human. This is going to become standard practice as AI evolves, or at least it should be, the WellSky rep told us. Machine assistance is far removed from machine perfection. Nevertheless, she asserted, few changes are required by the reviewer, usually a QA nurse.
Beyond OASIS
In addition to streamlining the OASIS assessment visit, the new app gives voice reminders to each nurse of their daily and weekly schedule, and background information about each patient’s visit history, current condition, and goals.
But Wait, There's More
Our AI tour did not end at the WellSky booth. We lost count of the number of smaller companies that were demonstrating the exact same AI-assisted OASIS assessment. It was as though some unknown force ordered, “OK, everyone. It’s 2025. Roll out your Home Health AI functions.”
One of many
Roger is the name of one of the more evolved such apps, from the aptly named Roger Healthcare. We had interviewed co-founder Yunus Ansari several months ago and were impressed by the product’s progress since then. Like WellSky and the others, Roger claims 15-minute OASIS visits, 5-minutes routine visit notes, 2-minutes EMR syncing, and larger per-nurse patient caseloads without additional work time.
Where Do We Go From Here?
When used to replace the clinical expertise of physicians, nurses, CNAs, and even personal care assistants, it smacks of HAL, the renegade computer of 2001: A Space Odyssey. What we need to do as AI infiltrates more and more aspects of our lives, is constantly remind ourselves that it is only a tool, not a master.
# # #

Tim@RowanResources.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com