Interoperability: The Unreachable Dream
Interoperabilityby Kristin Rowan, Editor
Interoperability
The Unreachable Dream
Healthcare and care at home have been reaching for interoperability for decades. When I started working in the care at home industry, there was a learning curve for terminologies, abbreviations (oy! with the abbreviations already!), and the pain points experienced by agencies and vendors. Interoperability was at the top of that list. 2009, the first full year I worked in care at home, was the year Congress mandated EHRs and data exchange. The mandate did not accomplish much. Incompatible data structures limit post-acute care data to the most recent health event, not the patient’s full medical record.
Data Exchange

Following the EHR mandate, Congress continued to add regulations and rules to advance data exchange. Starting with HIPAA in 1996, interoperability advanced as follows:
Health Insurance Portability and Accountability Act ensures patient data stays private both within a healthcare system and during data exchange
Congress mandated the use of EHRs throughout healthcare
HITECH Act launched Health Information Exchanges (HIEs) that support secure exchange of information between health systems
Health Level 7 (HL7) designed a framework that establishes protocols for data exchange
Fast Healthcare Interoperability Resources (FHIR), an updated of HL7, enables processes in 84% of hospitals and 61% of clinician offices
21st Century Care Act allows patients to access their own medical information and requires developers to publish APIs and ensure all data in the patient health record is accessible through that API
Trusted Exchange Framework and Common Agreement (TEFCA) lists principles, terms, and conditions to standardize data
CMS Interoperability Framework pushes interoperability nationwide through improved data quality; advanced technology; data aggregation; and alignment of data, tools, and measures
Following the EHR mandate, Congress continued to add regulations and rules to advance data exchange. Starting with HIPAA in 1996, interoperability advanced as follows:
- Health Insurance Portability and Accountability Act ensures patient data stays private both within a healthcare system and during data exchange
- Congress mandated the use of EHRs throughout healthcare
- HITECH Act launched Health Information Exchanges (HIEs) that support secure exchange of information between health systems
- Health Level 7 (HL7) designed a framework that establishes protocols for data exchange
- Fast Healthcare Interoperability Resources (FHIR), an updated of HL7, enables processes in 84% of hospitals and 61% of clinician offices
- 21st Century Care Act allows patients to access their own medical information and requires developers to publish APIs and ensure all data in the patient health record is accessible through that API
- Trusted Exchange Framework and Common Agreement (TEFCA) lists principles, terms, and conditions to standardize data
- CMS Interoperability Framework pushes interoperability nationwide through improved data quality; advanced technology; data aggregation; and alignment of data, tools, and measures
Thirty Years Later
Despite the laws, regulations, frameworks, and mandates, interoperability is not much better than it was in 1996. I had an experience this year that both enlightened and infuriated me. I switched health insurance plans for a variety of reasons. My new plan didn’t cover most of the doctors, hospitals, and health systems I had been using for many many years. So in February, I found a new PCP and had the standard start of care visit to establish my health history: current conditions, past conditions, past surgeries & procedures, current medications, etc. I requested referrals to new specialists and updates to prescriptions. My PCP performed a “complete physical” that was nothing more than a cursory overview. And then I waited.
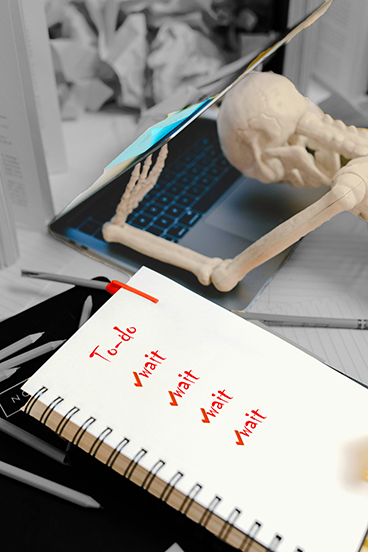
The Waiting Game
And waited…and waited…. I thought all these organizations and standards were supposed to make this easier. Still, I waited.
- I waited for an “invitation” to my PCPs portal to see my visit notes and test results
- I waited for my PCP to send referrals to new specialists
- I waited for my health insurance provider to inevitably tell me the specialist wasn’t covered under my plan
- I waited for a new referral from my PCP
- I waited for appointments, results, and recommendations
- I waited for access to new patient portals
- I waited for the portal to figure out how to give me access to three different providers in the same app
- (spoiler alert: I have to log in to the same app three different ways to access three different providers; my providers can see all the information in one place, but I can’t)
- I waited for test results to appear in each portal; some I had to call and request, some I’m still waiting for
Data Exchange "Advancements"
According to my research, 84% of hospitals and 61% of clinicians are currently using FHIR, designed to improve interoperability between different health systems using standard data formats and APIs.
Last month I had an appointment. Correction: I thought I had an appointment for an imaging scan. I thought this because the scheduling nurse called me to confirm the appointment day, time, and location. When I arrived, the check-in nurse couldn’t find me in their system.
It wasn’t just that she didn’t see my appointment. No, it was that she couldn’t find me at all. (We later discovered it was still pending because the imaging department never confirmed the appointment after the scheduling nurse added it.)
She could see no current or future appointments. She could see no past appointments because they were booked a different way. She couldn’t find any record of me at all. You see, my record started in the next building over.
Error 404: Not Found
Every one of these facilities is in the same healthcare system. (Think ACME hospital, ACME imaging, ACME specialist doctor, and ACME lab) Every office is part of the same healthcare system and none of them can see each other’s information. ACME hospital can’t see the schedule for ACME imaging and can’t schedule imaging appointments outside the hospital. For that, I have to call ACME imaging.
- But wait! The doctor wrote my referral for ACME hospital, not ACME imaging. I need a new referral.
- But wait! Neither the healthcare system nor the specialist can write a new referral. My payer will only accept a referral from my PCP.
- But wait! My PCP has no idea what the referral is for, how it was written, or where it’s supposed to go because my PCP can’t access my records from the healthcare system.
This is advanced data exchange using FHIR, HIE, TEFCA, and QHIN. My health system uses our local HIE and CommonWell Health Alliance, an interoperability network designated as a federal QHIN. Apparently, this ensures the health system can share data with participating providers, but not with themselves.
Home Health is Even Further Behind the Curve
After so many years, so many advancements, and so many regulations, interoperability is no more “solved” than it was in 2009. Even the health systems that are using all the tools aren’t even internally interoperable.
Home Health has an even harder time attaining interoperability.
- It is more difficult for HHAs to access patient information, which usually has to be manually imported into the home health EHR
- Patient consent is required, but HHAs often deal with patients who don’t have the capacity to consent
- Despite the requirement of APIs, most health information is spread out across multiple systems and the HHA only get information from the referring facility
- Nearly 80% of HHAs use an EHR
- Only 28% of HHAs are electronically exchanging information with outside facilities
- Only 18% can integrate shared data into automated workflows
- HHAs did not receive the financial incentives that larger healthcare systems got to push interoperability
- TEFCA participation is not mandatory, slowing down the process of approving a data connection and exchange
Many legacy EHRs have met significant challenges moving into interoperability. Competitors in the space had no financial incentive to create standard languages and formatting designed to share information. HHAs are left with two choices:
The costly, time-consuming task of reviewing, selecting, and onboarding an entirely new EHR –or–
Piece together workarounds with multiple 3rd party or internal solutions haphazardly strung together to resemble interoperability
Time is Up
# # #


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com









