Hospice Hope
by Peggy Rattarree, Principle Product Manager, Curantis Solutions
Hospice HOPE
The importance of documenting symptom impact for patient-centered care
In hospice care, the focus isn’t just on treating symptoms; it’s on improving the quality of life for patients and their families. This is where Hospice HOPE takes center stage, emphasizing the importance of documenting symptom impact to deliver truly patient-centered care. By understanding how symptoms affect each patient’s physical, emotional, and psychosocial well-being, hospice teams can provide care that aligns with their unique needs and goals.
What is hospice HOPE?
In hospice care, every patient’s journey is unique. By actively tracking and documenting symptom impact, care providers can move beyond generic treatments and embrace a truly individualized approach that prioritizes what matters most to the patient.
Why documenting symptom impact matters?
Moves us to patient-centered care
Documenting symptom impact allows hospice teams to focus on what truly matters to the patient. Instead of simply addressing symptoms like pain, nausea, or fatigue in isolation, it provides a holistic view of how these symptoms affect the patient’s daily life. For example:
- Pain
- How does it limit mobility or the ability to participate in meaningful activities?
- Fatigue
- Is it preventing patients from spending time with loved ones?
- Nausea
- Is it reducing their ability to eat or enjoy meals?
By asking these questions and recording the answers, hospice providers can better tailor interventions to manage not just symptom management but the overall patient experience.
Improves communication across the care team
In hospice care, communication is everything. Documenting symptom impact ensures that every member of the interdisciplinary team (IDT), from nurses and physicians to social workers and chaplains, has access to the same comprehensive information.
This documentation:
- Creates a shared understanding of the patient’s condition
- Helps align the team’s goals with the patient’s priorities
- Reduces duplication of efforts and enhances care coordination
When everyone is on the same page, patients and families receive more seamless, cohesive care.

Supports compliance and quality standards
Regulatory bodies like CMS (Centers for Medicare & Medicaid Services) require hospices to document and monitor patient symptoms to ensure care quality. But beyond compliance, tracking symptom impact demonstrates a commitment to continuous improvement.
Documenting symptom impact allows hospices to:
- Identify trends and gaps in care
- Measure the effectiveness of interventions
- Use data to advocate for better resources or innovations in care delivery
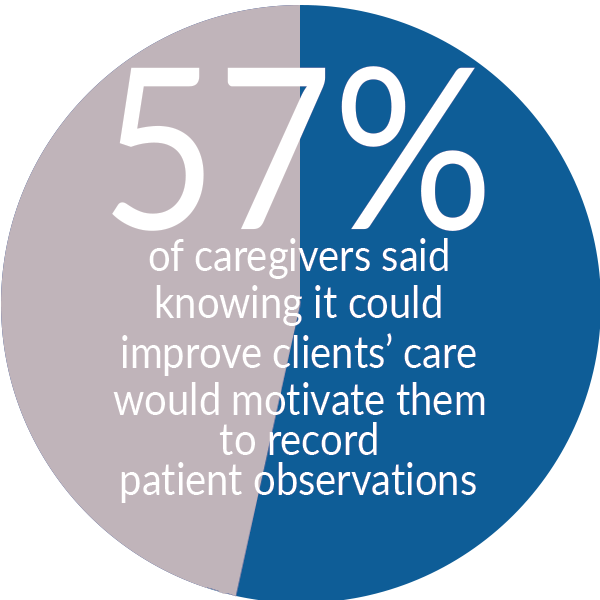
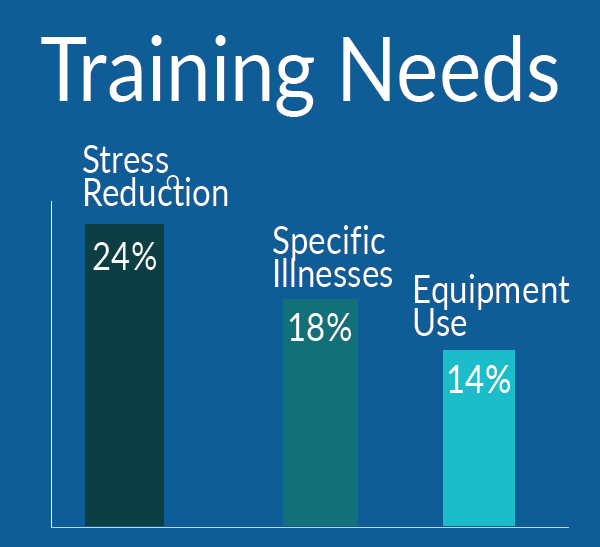
Empowers families and caregivers
When symptom impact is documented, families and caregivers gain a clearer understanding of their loved one’s condition. This transparency fosters trust and collaboration between the hospice team and the family, ensuring everyone is working toward the same goals.
For example, a caregiver might better understand why a loved one sleeps more during the day or avoids certain foods. These insights can help families feel more prepared and supported during a challenging time.
Final Thoughts
With CMS rolling out Hospice HOPE, documenting symptom impact is no longer optional. It’s the standard for compassionate, high-quality care. This shift helps hospice organizations go beyond symptom control and into whole-person care that honors each patient’s life journey.
This is part one in a two-part series on Hospice HOPE. Check back next week for part two.
# # #


Peggy is an IT professional with over 30 years’ experience. She has defined and developed software products in industries such as grocery management, financial services, and reporting and analytics. In her 2.5 years with Curantis, Peggy has helped to shape the definition and delivery of the application. She brings a passion for agility and has been integral in transitioning Curantis to an environment of delivery on cadence, release on demand.
Peggy has a Bachelor of Music degree from University of North Texas.
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in the Curantis Solutions blog and is reprinted here with permission. For more information or to request permission to print, please contact Curantis Solutions.