Situational Awareness Training
Adminby Lauren Rogers and Bobby McLain
Enhancing Safety Through Situational Awareness
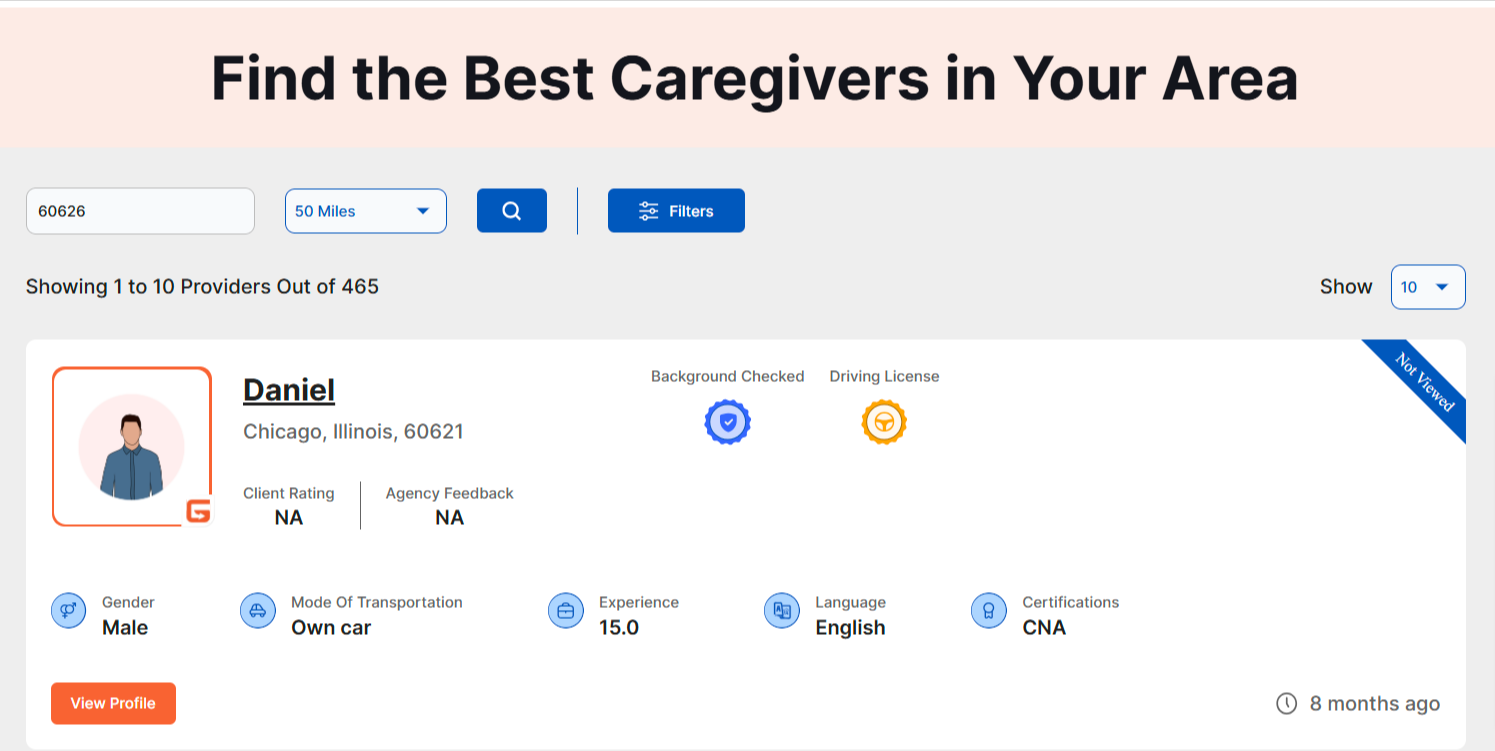
For home-health, hospice, and social workers, maintaining safety in unpredictable environments is crucial. Situational awareness is a key tool in ensuring personal safety and effective response to potential threats. It involves four main characteristics: observation, orientation, decision, and action. Here’s a brief guide on how to apply these principles in your daily work.
Observation
For home-health, hospice, and social workers, maintaining safety in unpredictable environments is crucial. Situational awareness is a key tool in ensuring personal safety and effective response to potential threats. It involves four main characteristics: observation, orientation, decision, and action. Here’s a brief guide on how to apply these principles in your daily work.


Orientation
Orientation involves understanding and processing the information you’ve observed based on your own experience and knowledge. Think about what is around you—consider the layout of the environment and how it affects your safety. If you find yourself in a difficult situation, where will you seek help? Familiarize yourself with exit routes and safe locations within the home or area.
Decision
Once you’ve gathered and processed information, it’s time to make decisions. Weigh your options carefully to determine the best course of action. Consider what you can do within your capabilities to mitigate any risks. Your decisions should aim to ensure your safety while also maintaining the well-being of those you serve.

Action
Action is the final step, where you use all the information and decisions you’ve made to execute a plan for safety. If you’ve identified a potential danger, act quickly and decisively. This might involve leaving the situation, calling for help, or using safety tools and protocols designed for emergencies.
Situational Awareness Final Thoughts
Applying situational awareness can significantly enhance your safety and effectiveness as a home-health, hospice, or social worker. By mastering observation, orientation, decision, and action, you’ll be better equipped to navigate challenging situations and ensure a safer work environment. Stay alert, make informed decisions, and take proactive steps to protect yourself and those you serve.
# # #

Lauren Rogers serves as the Director of Healthcare at Katana Safety, where she leverages her experience to enhance workplace safety in healthcare environments. She focuses on post-acute care providers and is dedicated to integrating innovative safety solutions that protect healthcare professionals.
She is passionate about creating safer environments, reducing risks for healthcare workers, and driving positive industry change. At Katana Safety, Lauren is committed to developing strategies that prioritize the well-being and safety of healthcare teams.

Bobby McLain is Chief Experience Officer for KATANA Safety, the Premier Provider of Lone and Workforce Safety Solutions. McLain’s previous roles include interim marketing leadership for multiple companies and executive positions at ScanSource, Inc., working in the company’s global marketing and strategic expansion efforts. McLain’s career began in event management and marketing, supported by a Bachelor of Arts in Journalism with a focus on Advertising/PR from the University of South Carolina. He can be reached at bobby@katanasafety.com or 864-630-9016 KATANA Safety: Never A Lone Worker
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com