Special Focus Program Ends
Advocacyby Kristin Rowan, Editor
Special Focus Program Not Well Received
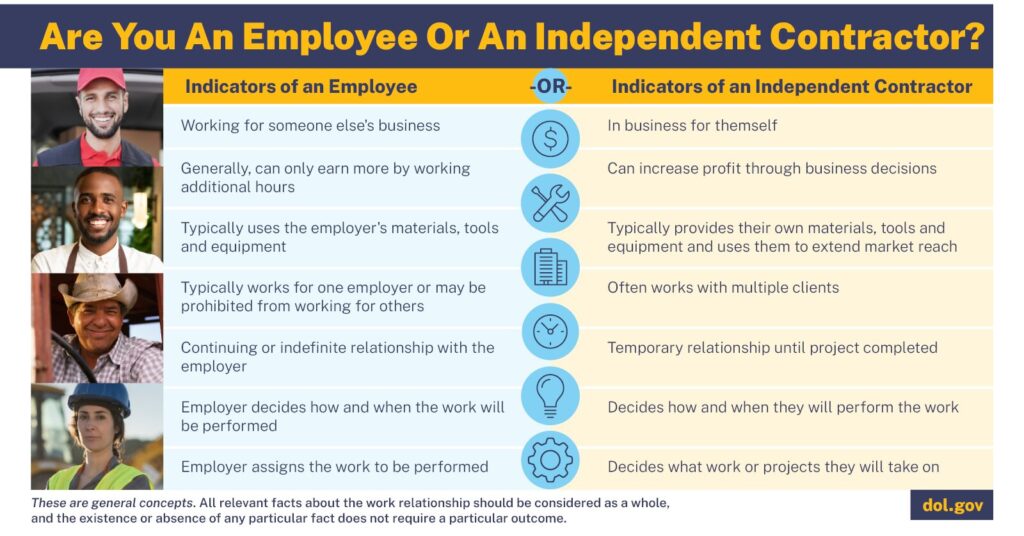
When the Hospice Special Focus Program (SFP) first appeared, the industry was told the program would help CMS identify and improve the performance of hospice providers that were struggling to meet quality standards. CMS developed the program to strenthen oversight, promote quality improvements, and ensure compliance for underperforming hospice agencies.
Soon after its inception and implementation in 2022, numerous concerns emerged. The National Alliance for Care at Home (then NAHC and NHPCO) voiced concerns over the program’s reliance on incomplete data as well as the potential for the program to unfairly targed providers in underserved communities.
Between February 2020 and January 2025, numerous state and national organizations have introduced Hospice Acts to Congress, given feedback to CMS on improvements to SFP, and filed lawsuits against the CMS.
Ramping Up the Opposition
In mid-2024, following the Council of States meeting, monthly opposition to the SFP became standard:
- The McDermott Report highlighted significant flaws in the algorithm used for the program. Again, there was an objection over the use of incomplete and inconsistent data.
- Bi-partisan Congress members sent a letter to CMS requesting revisions to SFP, criticizing outdated survey data and suggested that the quality metrics were inappropriately weighted.
- Alliance CEO Steve Landers publicly criticized the implementation of SFP in his op-ed.
- Representatives introduced Bill H.R. 10097 to delay SFP implementation, stating it would give CMS time to address the problems with the program and ensure fair application of standards for low-performing hospices without impacting quality programs.
- The Texas Association for Home Care & Hospice; Indiana Association for Home & Hospice Care; Association for Home & Hospice Care of North Carolina; South Carolina Home Care & Hospice Association; and Houston Hospice filed a lawsuit challenging the SFP as unlawful and arbitrary.
CMS Backs Down
This week, CMS announced that it has paused the implementation of SFP for the calendar year 2025. The CMS statement say the pause will allow CMS to “further evaluate the program.” There is no mention of the opposition or the ongoing lawsuits.
The hospice special focus program page on the CMS website reads:
Effective February 14, 2025, implementation of the Hospice Special Focus Program for CY 2025 has ceased so that CMS may further evaluate the program. Please contact QSOG_Hospice@cms.hhs.gov for policy questions.
All additional information about the program has been removed from the website page.
Special Focus Program gets First Positive Feedback
For the first time since 2020, industry leaders are applauding a CMS move regarding SFP. The move is halting the program altogether, but at least its positive feedback.
“This decision is a positive move acknowledging that the current approach is not working as intended. The hospice community has long advocated for strong oversight and patient protections, but the SFP, as implemented, was deeply flawed, unlawful, and harmful to the very patients it was meant to protect.”
You can read the full statement from The Alliance in their press release.
Final Thoughts
It seems it is not often that CMS hears what the industry tells them. Reimbursement rates continue to drop, documentation is increasingly complex, and the industry has suffered from their misconceptions about what we need. This time, at least, there was enough pressure and advocacy from Congress and from you, the people who are impacted daily by their decisions, to cause them to rethink this program. Keep up the good work and continue to advocate for yourself and for care at home. Perhaps this is not the last time CMS will listen.
# # #


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news .She also has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com