Workplace Violence in Home Health
Caregiver Safetyby Kristin Rowan, Editor
Workplace Violence and Policy Impact
Study of home health workers
A group of researchers from the University of Cincinnati, Ohio published a recent study¹ on the frequency and reporting procedures of workplace violence (WPV) in home healthcare. The study specifically addressed WPV in home healthcare, stating limited understanding of WPV in the home care setting. Most existing studies on WPV were hospital-based.
Frequency of Workplace Violence
Of the home health care workers (HHCW) surveyed, almost 37% responded that they experience both verbal and emotional violence in the workplace daily. More than 80% reported experiencing verbal aggression at some point. Physical violence is less prominent. 20% of respondants said they experience physical violence monthly. However, 56.6% said they have experienced physical violence at some point in their current agency. 76.6% of the time, the perpetrators of the violence are the patients of the HHCW.
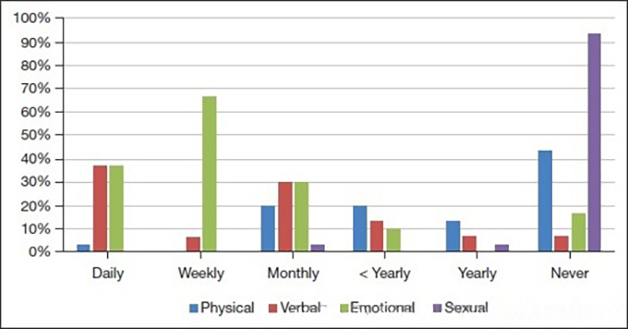
Fig. 1 Frequency of occurrence of physical, verbal, emotional, and sexual abuse as a function of time: daily, weekly, monthly, <yearly, yearly, and never.
Reporting Workplace Violence
All of the study participants indicated they had knowledge of workplace violence reporting procedures in their agencies, but 26.7% were unsure if the policies are contained in the employee handbook. 46.7% were uncertain as to whether the agency offered WPV or de-escalation training and 66% said prevention and de-escalation training was not mandatory. Unfortunately, 40% said their management did not encourage reporting and 33% said they were not comfortable approaching management about WPV. Despite the frequency of WPV among the respondents, none of the participants reported these incidents to management.
Thoughts
According to this, and other research studies on workplace violence in home healthcare, the problem is prevalent and persistent. Most HHCWs have experienced some sort of aggression, violence, or abuse in the course of performing their jobs. Of those who have, most do not report the incidents to management. Most HHCWs have not been trained in prevention or de-escalation. Even with training, HHCWs need a way to get immediate help. Unfortunately, most do not have an emergency alert system on their person during home visits.
Solution
Care at Home agencies, including non-medical supportive care, home health, hospice, and any other lone workers who are visiting patients in their homes, need safety policies and procedures. Agencies must include the same in the employee handbook, explain during orientation, and make available to HHCWs digitally.
Policies and procedures should include:
- A safety committee comprised of management, back office staff, and field workers
- A clearly written policy regarding physical, emotional, verbal, and sexual abuse
- Against a patient or their family/friends by a HHCW
- Against a HHCW by a patient or their family/friends
- Against a HHCW by a colleague or manager
- Against a HHCW by the environment in which they work (i.e. aggressive pets, weapons, cigarette smoking indoors, etc.)
- A digital reporting system that employees can use without having to approach management individually
- A clearly written policy on the management response to violence reporting
- A clearly written policy forbidding any retaliation or discrimination against a reporting employee
- Required research about new patients including
- Background/History of violence and/or mental instability
- Neighborhood safety rating
- Family members likely to be in the home and their history of violence and/or mental instability
Additional Tools for HHCWs
- Training in
- Violence prevention
- De-escalation
- Situational Awareness
- Self-defense
- A mandatory, GPS-enabled, multi-function safety device and platform to proactively manage caregiver safety and respond to incidents
- Optional escort service for new patients
- Mandatory escort service for new patients with a history of violence, mental issues, or incarceration
Workplace violence against HHCWs is not “if,” but “when.” It is the responsibility of the agencies to lower the risk, lower the percentage of “whens,” and encourage reporting. If you’re not sure how to begin, hire a consultant to help you build your safety committee and write your policies. It doesn’t matter how you start implementing safety protocols, as long as you follow through and protect your employees.
# # #


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
1. Obariase, E.; Bellacov, R.; Gillespie, G.; Davis, K. (2025). Assessing Workplace Violence and Policy Impact: A Cross-sectional Study of Home Healthcare Workers. Home Healthcare Now, 43(3), 150-156. doi: 10.1097/NHH.0000000000001345













