WellSky® and Ava Launch Groundbreaking Solution to Combat Staffing Crisis for Home-Based Care Agencies
The new innovation helps improve healthcare employee retention and engagement through incentive-based rewards
WellSky, a leading health and community care technology company, today announced the release of WellSky TeamEngage powered by Ava, a new innovation for home-based care providers aimed at increasing employee retention, reliability, and recruitment through gamification. The solution incentivizes and rewards caregivers for completing targeted activities and achieving performance goals, fostering a culture of appreciation while improving staff retention rates and agency differentiation.
WellSky TeamEngage
The solution comes at a time when home-based care providers face a growing workforce shortage crisis. The turnover rate for home care providers is 77%, challenging agencies to meet a growing demand for services with a shrinking supply of caregivers. This can result in higher rates of referral and client case rejection. With WellSky TeamEngage, agencies can implement customizable, data-driven incentives to attract and retain talent at scale, while shifting focus toward other operational priorities and providing exceptional care.
Using WellSky and Ava’s integrated technology, Griswold — one of the country’s largest home care franchises with more than 170 locations in 32 states and over 9,000 caregivers — reduced the turnover rate in its eight company-owned offices by 13% in just seven months and helped a large majority of caregivers reach key goals, such as clocking in and out on time and meeting minimum weekly hour requirements. The company has since rolled out the technology to its franchise network and expects significant adoption.
“We have seen tremendous benefit from using WellSky TeamEngage powered by Ava, both in the retainment of talented staff members and in the differentiation of our agency,” said Caitlin Griffith, Director of People & Culture at Griswold. “Our organization believes that care professionals are the foundation of our success, with innovation being key to improving the lives of those we serve. We have been pleased with the adoption and staff satisfaction with the solution, and we look forward to further benefiting from a comprehensive set of insights to guide our approach to workforce engagement strategies.”
Ava acts as an AI-powered Chief Engagement Officer
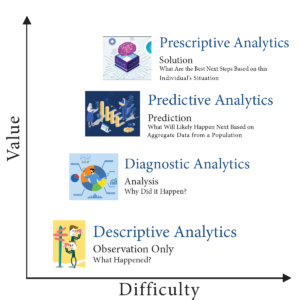
Its average customer improves employee retention rates by 45% in six months. Ava improves employee engagement so healthcare providers and administrators can redirect attention to scaling their businesses. Now in partnership with WellSky, the organizations will extend this technology to providers across the U.S., with the Ava platform integrated within WellSky electronic health records (EHR) technologies and the WellSky TeamInsights solution. TeamEngage will provide a comprehensive flow of data between systems and a seamless end-user experience.
“Ava works to remove the burden of administrative work and reconnect caregivers and home care administrators with why they chose a healthcare career in the first place,” said Victor Hunt, chief executive officer and co-founder of Ava. “We are excited to lend Ava’s Enterprise AI technologies to TeamEngage and, in doing so, tackle one of the greatest crises facing healthcare.”
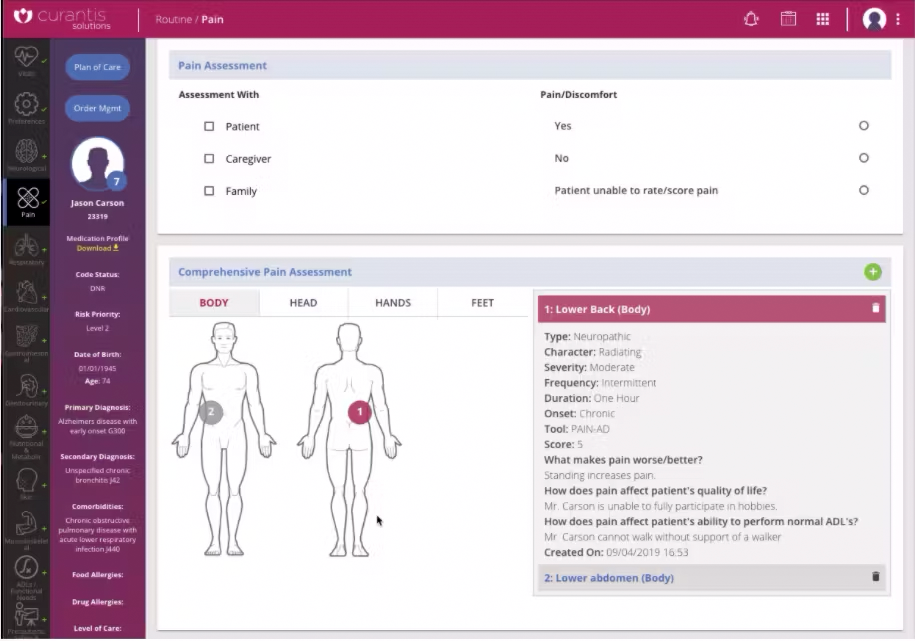
Leveraging data directly from WellSky Personal Care
WellSky TeamEngage incorporates specific caregiver actions, such as taking open shifts and performing timely clock-ins, into the agency’s defined incentive model, which stores all actions and awards points that caregivers can redeem for monetary or other agency-defined rewards. These day-to-day behaviors combined with pulse survey results, gamified referrals, and other engagement metrics are all tracked within WellSky TeamInsights for Personal Care, where powerful algorithms help predict caregiver turnover risk to proactively guide retention strategies.
“The staffing crisis facing our clients and the industry at large is a major concern, both for people seeking care in the home and for agencies trying to meet that need,” said Wes Little, chief analytics officer at WellSky. “We are thrilled to bring WellSky TeamEngage to our clients to not only provide them a tool to incentivize and reward caregivers, but to also gain the insights needed to run their operations at scale in today’s challenging environment.”
To learn more about how WellSky is powering agency staff retention and engagement, visit WellSky.com.
About WellSky®
 WellSky is one of America’s largest and most innovative healthcare technology companies leading the movement for intelligent, coordinated care. Our proven software, analytics, and services power better outcomes and lower costs for stakeholders across the health and community care continuum. In today’s value-based care environment, WellSky helps providers, payers, health systems, and community organizations scale processes, improve collaboration for growth, harness the power of data analytics, and achieve better outcomes by further connecting clinical and social care. WellSky serves more than 20,000 client sites — including the largest hospital systems, blood banks, cell therapy labs, home health and hospice franchises, post-acute providers, government agencies, and human services organizations. Informed by more than 40 years of providing software and expertise, WellSky anticipates clients’ needs and innovates relentlessly to build healthy, thriving communities. For more information, visit wellsky.com.
WellSky is one of America’s largest and most innovative healthcare technology companies leading the movement for intelligent, coordinated care. Our proven software, analytics, and services power better outcomes and lower costs for stakeholders across the health and community care continuum. In today’s value-based care environment, WellSky helps providers, payers, health systems, and community organizations scale processes, improve collaboration for growth, harness the power of data analytics, and achieve better outcomes by further connecting clinical and social care. WellSky serves more than 20,000 client sites — including the largest hospital systems, blood banks, cell therapy labs, home health and hospice franchises, post-acute providers, government agencies, and human services organizations. Informed by more than 40 years of providing software and expertise, WellSky anticipates clients’ needs and innovates relentlessly to build healthy, thriving communities. For more information, visit wellsky.com.
About Ava
 Ava is an enterprise AI platform helping healthcare providers streamline administrative busywork so that they can get back to care. In an industry where employee engagement and retention are crucial yet increasingly challenging to maintain, Ava provides an effective AI-driven solution that’s beneficial for clients, caregivers, and providers. Integrating seamlessly with Electronic Health Records (EHRs), Ava offers an engaging experience for caregivers and clinicians while providing administrators with a robust suite of tools for business intelligence, employee management, and gamified incentives. For more information, visit joinava.com.
Ava is an enterprise AI platform helping healthcare providers streamline administrative busywork so that they can get back to care. In an industry where employee engagement and retention are crucial yet increasingly challenging to maintain, Ava provides an effective AI-driven solution that’s beneficial for clients, caregivers, and providers. Integrating seamlessly with Electronic Health Records (EHRs), Ava offers an engaging experience for caregivers and clinicians while providing administrators with a robust suite of tools for business intelligence, employee management, and gamified incentives. For more information, visit joinava.com.
WellSky Media Contact
Emma Neal
Phone: 617.401.3131
Email: emma.neal@allisonworldwide.com
Ava Media Contact
Deanna Carbone
Phone: 914.523.7865
Email: ava@hirschleatherwood.com