Employee vs Independent Contractor
by Kristin Rowan, Editor
Follow the Rules
The very nature of care at home lends itself to different organizational structures. Hourly vs. per visit compensation. Employee vs. independent contractor. Shift work vs. standard schedules. Each decision can have its own advantages and disadvantages.
Two agencies were in the news this week after the Department of Labor determined they had misclassified employees as independent contractors and failed to pay overtime wages. In addition to back wages, these agencies were ordered to pay damages and civil penalties.
The Rowan Report has researched the 2024 Department of Labor Final Rule: Employee or Independent Contractor Classification Under the Fair Labor Standards Act, RIN 1235-AA43. We’ve provided our synopsis below to help you determine the classification of your workers to avoid similar penalties.
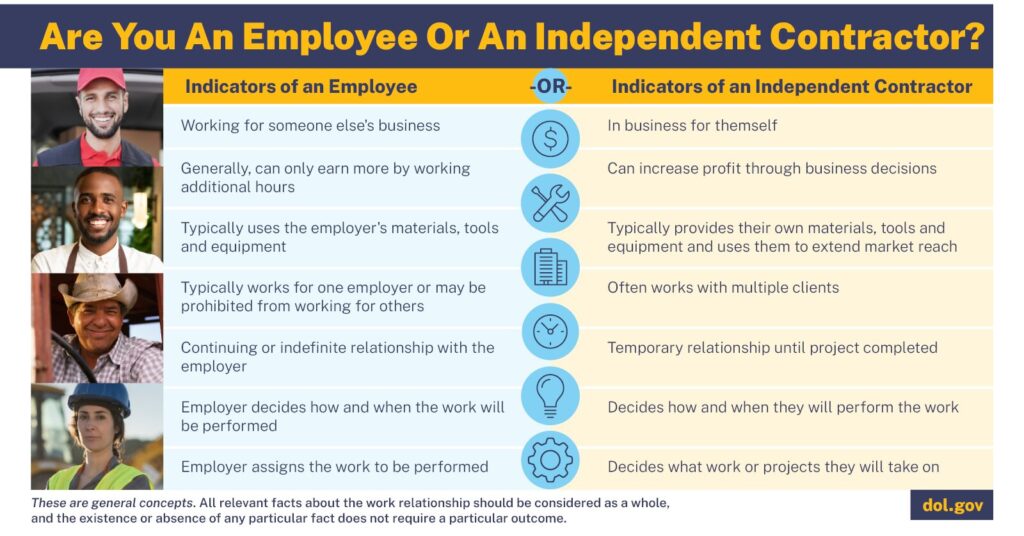
Employee vs Independent Contractor
The Fair Labor Standards Act, from the Department of Labor provides information on how to classify workers. Prior to 2021, the DoL used the economic reality test, used by courts to determine status. This test used economic factors including nature and degree of control over work, and the worker’s opportunity for profit or loss. These two factors weighed more heavily than the remaining three: the amount of skill required, how permanent was the relationship between the worker and the employer, and whether the work is part of an integrated unit of production (meaning all work leads to the same end product that cannot be completed without each person’s part.)
Totality of the Circumstances
Because the courts openly admitted that the final three factors would likely never outweigh the first two, the DoL moved to establish a different rule, using the five factors to determine a “totality of circumstances” without the predetermined weight. It also bent the final factor to include the work being an integral part of the business, not of production. Also included is the discussion of how scheduling, supervision, price setting, and the ability to work for others are considered within the control factor.
This final change is what will impact most care at home agencies. As defined in the Final Rule (795.110(B)(1)), this factor considers whether a worker has control over their own profit or loss, has control over their own schedule, advertises on their own behalf to get more work, and generally engages in managerial tasks such as hiring, purchasing materials, and/or renting space for themselves.
Qualifying as an Employee vs Independent Contractor
-
-
Must have control over their own profit and loss.
-
- If a worker can choose to accept or deny and job offered through the agency, therefore making more or less money, they may be an IC.
-
-
Should be engaged for short-term projects with identified end dates.
-
- This is vague in relation to care at home. An employer could argue that each home visit is a short-term engagement. However, the worker might say that the opportunity is on-going with no end date.
-
-
Invests in the building of their business.
-
- If a worker uses all their own equipment, is free to take shifts or jobs from other agencies, and promotes their skills in order to attract more work from outside your agency, they are likely an IC.
- If, however, the worker takes shifts from other agencies and promotes their skills to others because your business has predictable down-times, rather than of the worker’s own choice, they are likely an employee.
-
-
Should have control over multiple aspects of the job.
-
- A common misperception is that if an employee controls their own schedule, they are automatically an IC. Many employees have flexible scheduling, work from home opportunities, and other controls over their schedule. Care at home workers make less money when they choose to change their schedule, indicating economic dependency on the company. Further, many agencies have a minimum hour requirement with disciplinary action or consequences for not meeting that minimum. These factors, regardless of scheduling flexibility, mean the worker is not an IC.
- Nurses who have control over their own schedules do not control, for example, the rate they are paid for their services. When the employer controls prices for services, workers are likely employees.
- How a job is performed should be a considerable factor. If the worker is free to determine how they actually do the work once they take a job, then they are likely an IC. This may be possible for non-medical supportive care at home, but is less likely for home health and hospice settings that are highly regulated.
-
-
Should not be supervised either in person or by technology, using a device or other electronic means. Ongoing and continuous supervision is not required to classify a worker as an employee, only that the employer maintains the right to supervise. Supervision in this case is not limited to watching the worker during a shift. Supervision also includes training and standards established during hiring, remote monitoring of a job using an electronic visit verification system, and/or the oversight of completed work in the case of a QA audit of documentation.
-
- For home health and hospice agencies, this almost assuredly makes all nurses employees. However, exceptions may exist in the case of specialties such as wound care, physical or occupational therapy, ostomy care, and respiratory care.
- For non-medical care at home, this factor should be weighed based on your agency’s protocols.
-
-
Must be able to work for others.
-
- An employer who limits a worker’s ability to work for other agencies and/or put such constraints on a person’s schedule as to make it impossible to work for others has employees, not ICs.
- Non-compete clauses and fines for taking clients outside of the agency point to employee status.
- Working part-time and having the ability to work for another company, also part-time, does not necessarily make someone an IC.
-
-
Should not be an integral part of the business.
-
- If the business cannot function without the service performed by the worker, the worker is an employee.
- Similarly, if the work itself depends on the existence of the business, the worker is an employee.
- Generally speaking, if a the primary business is to make a product or provide a service, then any worker involved in making that product or providing that service is integral to the business.
- This final clarification from the DoL may require all care at home workers to be classified as employees.
-
-
Implications for the Industry
If most care at home workers should be classified as employees, not independent contractors, you should expect to make significant changes if you currently have your workers classified as ICs.
- Higher expenses in the form of taxes and benefits
- Negotiations for paid vacation, personal, and sick leave
- Potential auditing of prior business structure and classification
- Complete overhaul of back-office hiring processes and software needs for onboarding employees instead of independent contractors
Employee vs Independent Contractor Corrective Action
- If your workers are misclassified as independent contractors, take steps to correct this effective January 1st so your new tax year is correct.
- Plan ahead to incorporate required taxes coming from your budget.
- Determine whether you may have workers who are owed back wages, overtime pay, or other benefits and take steps to rectify the situation before you end up on the Department of Labor radar.
Final Thoughts
I’ve heard a lot of conversations from home health and non-medical supportive care agency owners about the policies they have in place for their caregivers. The new laws around non-compete clauses as well as this updated Independent Contractor test leads me to this conclusion:
Most workers in care at home are employees, not independent contractors. If you wish to classify your workers as independent contractors, do your research, reorganize your business, and make sure you are following the totality-of-the-circumstances test.
If organizational change is not possible, look at transitioning your workers to employees before the start of the year and hire a consultant to help you with the changes you need to make.
# # #


Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com