Agency Management System for Fractional Home Care
by Tim Rowan, Editor Emeritus
Agency Management System for Fractional Home Care
There is a growing service sector within Home Care to provide in-home care to seniors living in Independent Living and Assisted Living facilities. We described the basics of the way it works in last week’s interview with Jessica Nobles. She pointed out that there was no software available for the kind of scheduling required by this type of home care. She wound up creating her own software to schedule on-site caregivers performing visits that can be anywhere from five-minutes to full, four-hour shifts.
Right after building the customized scheduling tool, Ms. Nobles met Tim and Gina Murray, who had been through an identical experience with their own agency, Aware Home Care. The difference between their stories was that both the Nobles’ and the Murray’s, after selling their respective agencies, embarked on different paths. Jessica and Clint went the consulting route and Tim and Gina formed a software company, CinchCCM, Community Care Made Easy. We spoke to them this week to hear the rest of the story.
Agency Management System Win-Win-Win
At no cost to the residential facility itself, a home care agency places one or more caregivers on the premises. IL or AL residents join a kind of co-op to be eligible to request in-home services. Some agencies who offer this service accept requests for traditional shifts, five-minute check-ins, and pretty much everything in between.
Many request regular morning breakfast help, others tuck-in services. Most agencies in this sector allow registered members to request unscheduled, as-needed help. To accommodate the needs of all members, an agency will add caregivers as the number of participants grows. The Murray’s outlined the benefits to all involved.

- Caregivers like predictable income. They are paid for their entire time on-site, whether they are in a member home or on call between visits.
- IL and AL owners find that the level of care keeps residents in their facilities longer by delaying the need to move to a nursing facility.
- Families gain peace of mind, knowing their older loved ones have a caregiver nearby and on call all day, sometimes overnight.
- Home Care agencies report enhanced caregiver satisfaction and retention, along with a steady, predictable payroll.
Clearly, agency management software was not intended to automate this type of arrangement.
Not Your Parents' Agency Management System
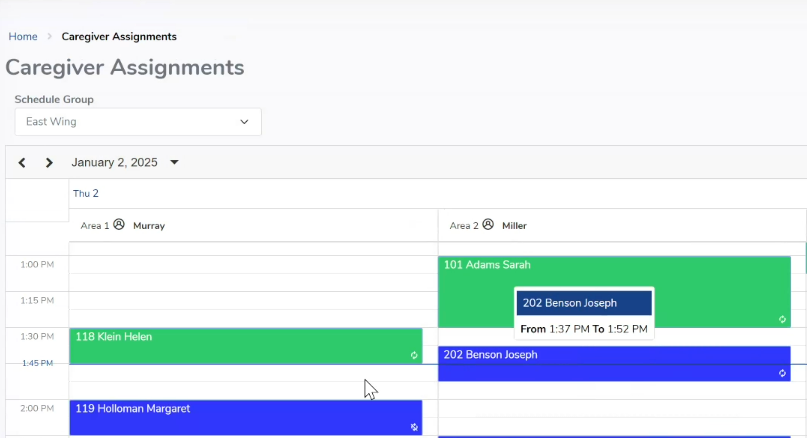
The Murray’s designed a system that displays schedules on a color-coded, calendar grid, with a column for each day and row for each 15-minute unit. Then they began to add features.
- caregivers can tweak scheduled visits by drag and drop
- remote family members can see scheduled and completed visits as well as caregiver notes
- on the system’s mobile app, each caregiver can see the schedule of all other on-site colleagues. If a client unexpectedly needs more time and a caregiver has another visit coming up, that caregiver can find an available colleague and ask, through a secure message on the app, for someone to fill in.
- on the system’s mobile app, each caregiver can see the schedule of all other on-site colleagues. If a client unexpectedly needs more time and a caregiver has another visit coming up, that caregiver can find an available colleague and ask, through a secure message on the app, for someone to fill in.
- a management dashboard displays real time charts of caregiver utilization and gross profit. Agencies with multiple sites can report each site’s data separately and roll all sites up into one combined report.
Tim Murray explained that version 5.0 is nearly finished and ready to be released later this year. “It has been a long, slow development process,” he said, “and the first version was functional but simple. Adding the mobile app was a big step forward and very popular with the field staff. Management reports and real-time charts brought CinchCCM from a scheduling application to a full agency management system.”
Pricing, Growth, Evolution
CinchCCM is priced per client, based on average daily census at the end of each month. The Murray’s found this policy to be both manageable and fair. Their customers have a predictable revenue stream if most residents choose the monthly retainer option, and they have a predictable software cost for budgeting.
As word spread and software sales grew, Tim and Gina Murray sold Aware Home Care, formed a corporation, and turned their efforts to feature development, customer support, and sales. Those efforts have led to growth to 60 clients across the country. “As the so-called fractional home care concept grows,” Gina Murray concluded, “we want to be there to make it a smooth experience for those who give it a try.”
# # #

Tim Rowan is a 30-year home care technology consultant who co-founded and served as Editor and principal writer of this publication for 25 years. He continues to occasionally contribute news and analysis articles under The Rowan Report’s new ownership. He also continues to work part-time as a Home Care recruiting and retention consultant. More information: RowanResources.com
Tim@RowanResources.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com