Medicare Advantage Lowers Home Health Care Use
by Kristin Rowan, Editor
End-of-Life Care in Medicare Advantage vs Traditional Medicare
Using research from CMS, researchers from Mt. Sinai in New York and Brown University in Rhode Island studied the data of adults aged 66 and older who passed away and had Medicare coverage in their final year of life. Included in the study were people potentially eligible for home health care and not in a nursing facility, hospital, or hospice care setting. Data from close to 1.8 million people was analyzed. The researchers identified whether the participants received home health care and how many days of end-of-life care they received.
Home Health Higher in Traditional Medicare
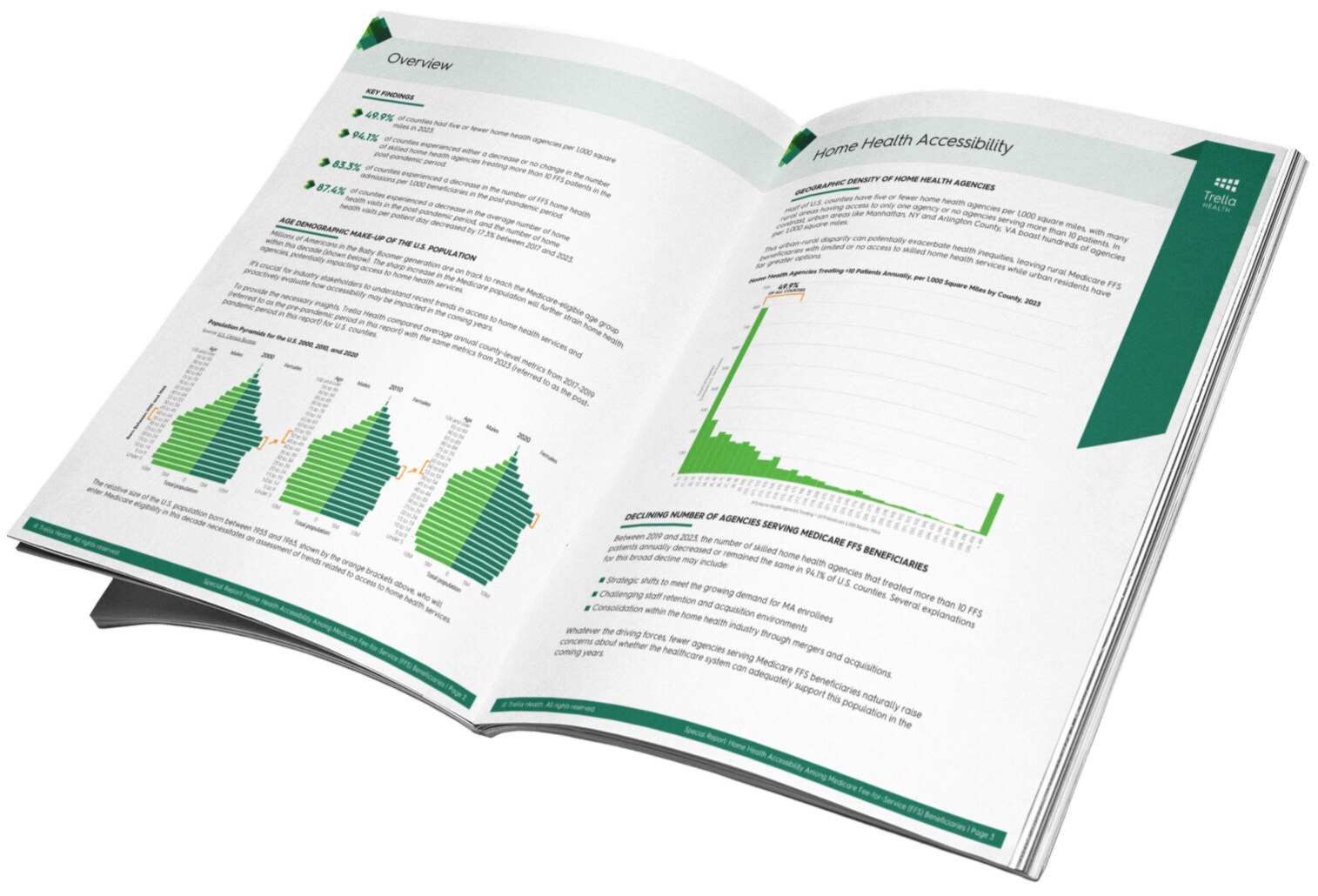
Of the nearly 1.8 million participants, the average age was 82. 51.5% were female and 36.5% were enrolled in Medicare Advantage. In the final year of life, home health care use was recorded at 37.5% for MA enrollees and 41.7% for traditional Medicare.
When the researchers looked at different demographic groups within the data sets, home health care usage was higher in traditional Medicare in most groups. However, among American Indian and Alaska Native groups, Medicare Advantage had a slightly higher rate of home health use at 37.9% compared with 37.1% in Traditional Medicare.
Conversely, in the Asian or Pacific Islander demographic, home health use rate was 32.6% in MA and 41.8% in TM. Similarly, the rate of use among the Hispanic group was 33% in MA and 44% in TM. Following a similar trend, in the non-Hispanic Black group home health usage in MA was 38.8% compared with 42.9% in TM. Likewise, among the non-Hispanic White group, home health use in MA was 37.9% versus 41.5% for TM. For those of unknown race, usage was 36.1% in MA compared with 40.1% in TM.
Days of Care Lower in Medicare Advantage
Home health users across all racial and ethnic demographic groups enrolled as Medicare Advantage beneficiaries had fewer days of care in home health than those enrolled in Traditional Medicare. The stand-out group in this part of the research was those of Hispanic descent, who averaged 81.9 days in home health care in Medicare Advantage compared with 111.9 days in Traditional Medicare.

Implications
The researchers indicated some limitations in the study, namely that data was pulled from pre-covid patients because of the changes in home health during covid. The study should be repeated with post-covid data. One of the researchers received personal fees while serving as a senior advisor to CMS. Another received personal fees as a section editor for UpToDate. A third researcher reported receiving personal fees from Abt and UpToDate.
Despite these limitations, the implications of the study show that end-of-life care is not the same between Medicare and Medicare Advantage patients. Medicare Advantage is largely operating on a Value-Based Purchasing Model. The fewer services the beneficiary receives, the more money the primary doctor, hospital, and payer keep. It is not surprising, therefore, that MA patients get fewer services for less time. Patients who switch from Traditional Medicare to Medicare Advantage, especially if they are your patients, should be informed that they are still eligible for home health care and hospice care, but they may have to ask for it.
# # #


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news .She also has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com