by Kristin Rowan | Sep 4, 2025 | Advocacy, Regulatory
In 1938, the Fair Labor Standards Act (FLSA) established a federal minimum wage, guaranteed overtime, and kept children out of the workforce. Exemptions to FLSA include executive, administrative, professional, computer employee, and outside sales positions. Employers did not pay minimum wage for retail workers, service workers, agricultural workers, or construction workers.
Domestic workers included
An amendment to FLSA in 1974 added domestic workers to those who must receive minimum wage and overtime. The amendment did not include “companionship services” and live-in domestic service employees. A later amendment from 2013 narrowed the definition of “companionship services.” This eliminated the exemptions for workers who provided “care.” Companions could still be exempted from overtime. This stopped home care agencies from claiming exemptions and required overtime pay for home care workers.
The Department of Labor is considering unraveling the 2013 amendment. There is a concern that they may have misinterpretated the rule. Additionally, requiring overtime for home care workers will increase the cost of care. Supporters of the rule change believe that allowing exemptions for overtime among home care workers would make live-in care more affordable. If the 2013 amendment is removed, employers would not have to guarantee minimum wage or overtime for home care aides.
The DOL argues that this change will make care more affordable and expand access to care at home. However, there is already a workforce shortage in the industry. Lowering pay rates and removing overtime could cause a mass exodus from the industry. As far as we know, DOL did not discuss requiring CMS to increase reimbursements rates or covering non-medical supportive care at home as an alternative.
“Removing basic labor protections from home care workers will only exacerbate the multiple issues buffeting the home care sector, its workers and consumers: serious threats from cuts to federal Medicaid contributions, changing immigration policies and the lack of realistic long-term services and supports (LTSS) options.”
President and CEO, LeadingAge
Comments from the industry
The public comments period on this proposed rule change ended on September 2, 2025. The proposed rule received roughly 5,300 comments. Some examples of feedback include:
“…reversing the 2013 protections, the DOL would undermine the wages and economic security of home care workers…exacerbate turnover and workforce shortages…[and] harm older adults and people with disabilities….” – Hand in Hand: The Domestic Employers Network
“This proposed change is a crucial step toward restoring flexibility and affordability in home care services, particularly for families relying on live-in support.” – Owner, Home Helpers Home Care of Larimer County and member of HCAOA and IFA
“…strongly support workforce development and has historically and continues to support thoughtful solutions to our workforce crisis. We strongly support the restoration of the overtime exemption.” – The Virginia Association for Home Care and Hospice and the West Virginia Council for Home Care and Hospice
“Home care workers are also strongly vital for companion care, personal care, home health, nursing, therapy, caring for the disabled and the elderly, and more. The proposed rule that was meant to strip home care workers of wage and overtime protections is absolutely cruel and harmful for home care workers…” – Derek Dinh, CA
“I am not a home care worker, but used a home care worker to take care of my mom when she was unable to do things around the home and then got progressively worse. They need to be paid a living wage and receive overtime. They are professional people who take care of those who need care.” – Wendy Peale, NY
- Among the people and organizations who have publicly expressed opposition to this change are:
- LeadingAge
- Autistic Self Advocacy Network
- American Civil Liberties Union
- Congresswoman Pramila Jayapal
- The Commonwealth of Pennsylvania, California, Colorado, Connecticut, District of Columbia, Hawaii, Illinois, Massachusetts, Maryland, Maine, Michigan, Minnesota, Nevada, New Jersey, New York, Oregon, Rhode Island, Vermont, and Washington
The has not issued a final rule. However, neither has the DOL enforced the requirement since July 25, 2025. Home care agencies can currently claim overtime exemptions. There is no set timeline yet for a final decision. We will continue to follow updates on this topic.
Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Kristin Rowan | Aug 21, 2025 | Legal, M&A, Medicare, Medicare Advantage
DOJ Settles with UnitedHealth and Amedisys
DOJ settles with UnitedHealth and Amedisys after almost nine months of negotiations. The Department of Justice (DOJ) initially blocked the proposed merger between UnitedHealth and Amedisys, citing concerns over eliminating competition in home health and hospice services in some areas of the U.S. After the most recent settlement hearing, the merger seems to be back on track.
Public Comment Period and Judicial Review
Now that the DOJ hurdle has been passed, there is a public comment period. Following the public comment period, the U.S. District Court for the District of Maryland will enter final judgement. From the Justice Department website:
As required by the Tunney Act, the proposed settlement, along with a competitive impact statement, will be published in the Federal Register. Any interested person should submit written comments concerning the proposed settlement within 60 days following the publication to Jill Maguire, Acting Chief, Healthcare and Consumer Products Section, Antitrust Division, U.S. Department of Justice, 450 Fifth Street NW, Suite 4100, Washington, DC 20530.
Antitrust Division Statement
“In no sector of our economy is competition more important to Americans’ well-being than healthcare. This settlement protects quality and price competition for hundreds of thousands of vulnerable patients and wage competition for thousands of nurses. I commend the Antitrust Division’s Staff for doggedly investigating and prosecuting this case on behalf of seniors, hospice patients, nurses, and their families.”
Assistant Attorney General, Justice Department Antitrust Division
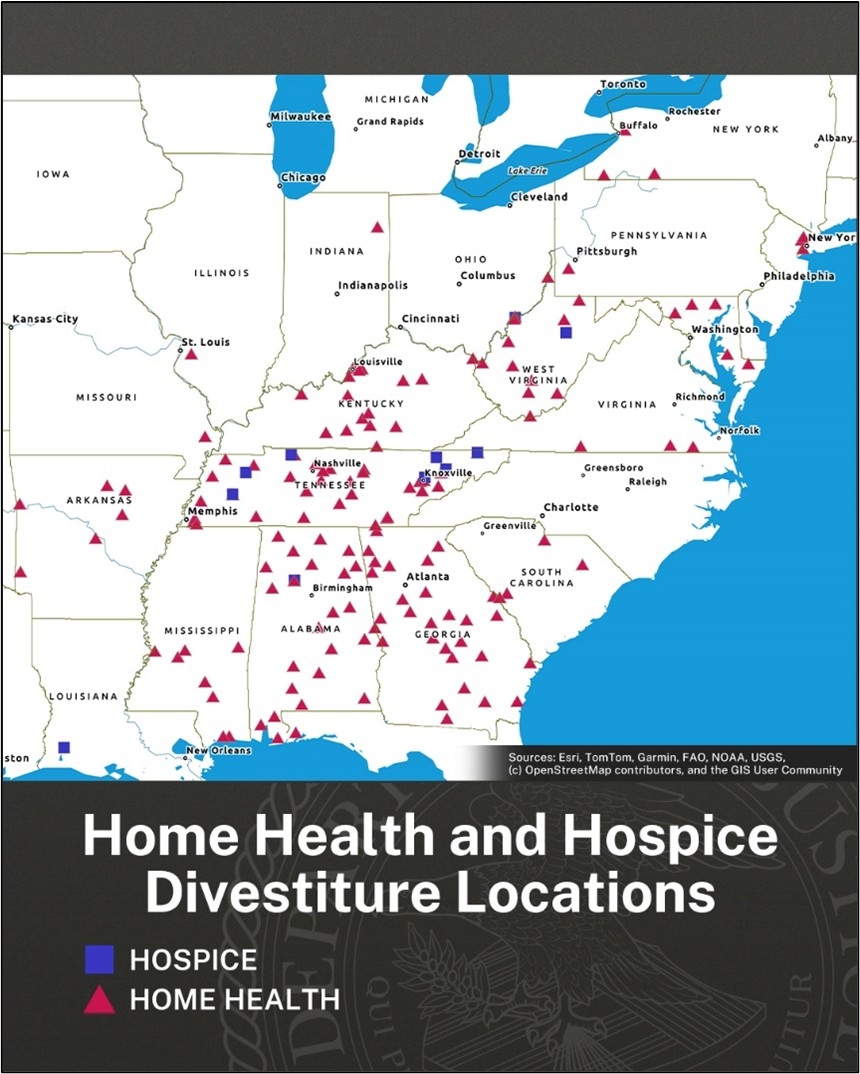
According to the new agreement, UnitedHealth will sell 164 home health and hospice locations across 19 states. In addition to the sale, the agreement provides the buyers of these locations with assets, personnel, and relationships to help them compete with remaining UnitedHealth locations. Also included are protections to deter UnitedHealth from interfering with the new owners’ ability to compete.
BrightSpring Health Services and Pennant Group will acquire the 164 locations. Slater said the settlement, which includes the largest ever divestiture of outpatient healthcare, protects quality and price competition patients as well as wage competition for nurses. However, antitrust specialist Robin Crauthers, a partner with McCarter & English, says it doesn’t go far enough. According to Crauthers, the settlement agreement does not address all of the markets that would have less competition and that the DOJ accepted less than they wanted in the agreement.
Additionally, critics argue the divestiture moves 164 home health and hospice agencies from one large player to two other large players in the space. Arguably, rather than preserve competition, this divestiture agreement will only serve to strengthen the largest players in the market, giving them a substantial advantage over smaller agencies in these areas.
Joe Widmar, Director of M&A at West Monroe consulting firm, says that the number of home health and hospice agencies is not the tipping factor in competition. Rather, it is UnitedHealth’s vertical integration. A health insurance company that also owns nearly 2,700 subsidiaries, including pharmacies, home health and hospice, behavioral health, consulting for healthcare organizations, surgery centers, hospitals, mental health, managed care for Medicaid and Medicare, and specialty care. Virtually any referral from a PCP to any other health professional puts more money into the health care giant’s pockets. The lack of competition is across all forms of healthcare, leaving patients no choice buy to support UnitedHealth Group in areas where all local healthcare providers are subsidiaries. I 2024, UnitedHealth insurance paid $150.9 million to its subsidiaries for care. These provider companies are not counted in the profit caps placed on insurance companies.
In addition to side-stepping profit caps, vertical integration aids in upcoding. Upcoding is the practice of digging into a patient’s life to find (or create) additional patient needs. Insurers add as many codes as possible for the greatest reimbursement rates. According to a recent study, UnitedHealthcare overbilled Medicare Advantage by $14 billion through upcoding.
In-home health risk assessments and patient reviews, often offered to beneficiaries as a free service, result in an average risk score 7% higher than in patients seen in medical practices and hospitals. UnitedHealth generates more income from patient review diagnoses than any other MA insurer. The Department of Justice is currently investigating UnitedHealth’s Medicare billing practices.
If you own a home health, hospice, or palliative care agency in any of the states shown in the graphic above, write to Jill Maguire with comments and concerns. Our primary objective is providing quality care to patients in their homes. We know that home care is less expensive for the patient and government-funded insurance. But not when all the home care agencies in an area are owned by only a few of the largest home health agencies in the country. And not when the insurer is adding diagnostic codes to pad their bill.
Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Rowan Report | Jul 24, 2025 | Partner News
HHAeXchange Unveils New Corporate Headquarters in New York City
New location reaffirms the company’s commitment to its employees and customers with expanded office space to support enhanced collaboration, creativity, and innovation
NEW YORK, June 3, 2025 – HHAeXchange, a leader in homecare management solutions for providers, caregivers, managed care organizations (MCOs), and state Medicaid programs, today announced the opening of its new corporate headquarters in New York City.
Located in the heart of Midtown Manhattan, the reimagined workspace is a reflection of the company’s recent growth and its commitment to delivering advanced solutions for the home and community based services (HCBS) industry. The new space also marks an important step in uniting teams from HHAeXchange’s recent acquisitions of Sandata, Cashé Software, and Generations Homecare System. Efforts to foster stronger collaboration across functions will accelerate the delivery of a more connected, efficient experience for customers nationwide.
“We are always striving to better meet the needs of our customers, and bringing our employees together at our new headquarters will support greater collaboration that drives product innovation. New York has been our home base since 2008, and we’re proud to grow the HHAeXchange footprint locally while creating a welcoming work environment for our network of employees, customers, and partners from across the nation.”
CEO, HHAeXchange
For more than 15 years, HHAeXchange has been at the forefront of homecare technology, innovating software solutions that empower personal care providers, self-direction program administrators, MCOs, and state Medicaid agencies to achieve operational efficiency, increased compliance, and improved member outcomes. The new central office space reflects HHAeXchange’s focus on supporting its teams and customers, helping to advance care delivery for all members.
In addition to the office’s collaborative workspace, HHAeXchange’s new headquarters features state-of-the-art employee training rooms and flexible meeting spaces designed to foster engagement with customers, prospective clients, and partners.
We sat down with Paul Joiner, CEO of HHAeXchange, to talk about the new office space, how its impacting the company culture, and what’s next for the company. See our accompanying article here.
by Kristin Rowan | Jul 24, 2025 | Admin, Artificial Intelligence, Home Health, Hospice
Paul Joiner, CEO of HHAeXchange, sat down with The Rowan Report Editor Kristin Rowan to discuss the company’s new headquarters in Manhattan, the company culture he’s creating, his dedication to support those helping our most vulnerable populations.
The Rowan Report: Paul, thank you for taking the time to talk to us. HHAeXchange is going through some significant growth recently. And now you’ve moved your headquarters from Long Island to Manhattan, correct? How did that decision come about?
Paul Joiner: HHAeXchange has been in Manhattan for a long time. Sandata, who we acquired earlier this year, was in Long Island. But, the move was planned with or without Sandata. We needed a nice sized space to convene people. We valued a large, multi-purpose meeting space over individual office space. It’s a space where the teams can meet when they come to town, where we can host clients, and larger company meetings.
RR: How does the new space support your team?
Paul: The majority of our team is remote. I don’t think remote work is healthy for everyone. It varies from person to person. It’s not a long-term healthy option. Returning back to the office 9-5 five days a week isn’t practical and not all that healthy either. We have created policies, a workspace, and a culture where people are invited to visit. Some come 2-3 days per week. Some only once a month. We maintain flexibility for our teams to work when and where they need to work. Being a single parent, for example, is really hard, so we stay flexible to support single parents to be where they need to be.
At the same time, we’ve seen the benefit of the connection and how much more healthy it is by physically coming together. For the younger workforce, they are enjoying getting together and coming into the office. We have to support our younger employees and their professional development. How do you professionally develop via Zoom or Teams? Physically coworking and promoting good and active environments compel people to come into the office. To build connections, you have to be together, not just on video.
RR: You have workers across the country, though. How does that work?
Paul: We have the main office here in Manhattan, a large and growing office in Minneapolis, and a smaller office in Miami. We try to keep people in areas that make it easy to meet. However, we do have some roles with certain criteria that allows for mostly remote work. Those teams come to one of the offices to meet when they can. We’ve hosted team meetings here and in Minneapolis recently.
RR: Has this new meeting space had an impact on the company culture?
Paul: Yeah, it has improved. We are having real, honest conversations about what needs to be improved. The team effort is the way we win and our teams understand that. We also understand that working hard doesn’t mean foregoing your life and the ability to recharge.
Work hard, be passionate, and motivate people with your mission and vision. The people we serve don’t have it easy, they are supporting the most vulnerable people.
RR: In a recent statement, you said that the new location will support collaboration and innovation. Do you have new features on the horizon? Are you investing in AI capabilities?
Paul: We have a lot in the works. We have a new mobile app in the beta phase that we’ll be rolling out that I’m really excited about. It’s actually an update, but it’s so massive that it’s basically new. We’re working on data analytics and data tracking for some of our largest clients. We’ve consolidated some screens into one spot to streamline and make the user more efficient. A lot of what we’re working on is foundational. We’re focusing on supporting companies as they scale.
RR: Are you looking into AI, either within the HHAeXchange platform, or in a partner?
Paul: Yeah, of course. AI is the future and it’s everywhere. We are looking at ways to return time to users, make it easier to train users, and make things easier on caregivers. We will try to generate more buzz around AI, but not until there’s real, tangible value. AI definitely needs to be part of our strategy, but being smart where we apply it to truly get the value-add for our clients. It has to improve the quality of life for the user. Does it improve the ability of caregivers to care for people?
RR: Do you have any additional acquisition or growth plans for the second half of 2025?
Paul: There’s a lot going on in the marketplace right now. A lot of our clients are growing really well also. So, we’re sort of in a heads-down mode. There’s a handful of things we’re looking at. Right now, I’m really excited about being a bigger participant across the full continuum of care for our populations. There are some opportunities to innovate and evolve to support integrated care over the next few years. I’ll just leave it at that…for now.
RR: Paul, thank you for joining me today. It’s always a pleasure.
Founded in 2008, HHAeXchange is the leading technology platform for homecare and self-direction program management. Developed specifically for Medicaid home and community-based services (HCBS), HHAeXchange connects state agencies, managed care organizations, providers, and caregivers through its intuitive web-based platform, enabling unparalleled communication, transparency, efficiency, and compliance. In 2024, HHAeXchange expanded through the strategic acquisitions of Sandata, Cashé Software, and Generations Homecare System, strengthening its commitment to advancing the industry.
Paul Joiner is an accomplished executive with extensive leadership experience in the healthcare sector. Currently serving as a Board Member at AssistRx, Joiner has held prominent positions, including Chief Executive Officer at both HHAeXchange and Kipu Health. Previous roles include Chief Operating Officer as well as Executive Vice President and General Manager at Availity, and Senior Vice President and General Manager of Health Plan. Joiner also served as Vice President of Client Engagement and Business Development at Midas+ Solutions, Xerox Healthcare Provider Solutions. Educational qualifications include a Master of Accountancy from Belmont University and a Bachelor of Accountancy from the University of Mississippi.
Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Rowan Report | Jul 26, 2024 | Partner News
Axxess 2025 AGILE Conference to be held May 5-7 in Dallas
DALLAS, July 18, 2024 – Axxess, the leading global technology innovator for healthcare at home, today announced the 2025 Axxess Growth, Innovation and Leadership Experience (AGILE) will be held May 5–7 at the Fairmont hotel in downtown Dallas.
Each year several hundred care at home thought leaders, industry providers and partners attend AGILE to learn and share insights to help build the future of healthcare at home. The conference also features valuable networking opportunities and educational sessions on topics at the leading edge of care at home. Clinicians earn much needed continuing education units toward their license renewal.
“AGILE is the must-attend event for anyone involved in care at home,” said John Olajide, Founder and CEO of Axxess. “We are excited about the future of care in the home and believe AGILE 2025 will play a crucial role in advancing our industry by fostering innovation and bringing our community together to learn and grow. Next year’s conference will feature thought-provoking keynote speakers, informative breakout sessions and interactive workshops, all focused on the latest trends, technologies and best practices. I know that AGILE 2025 will inspire and equip attendees with the knowledge they need to provide exceptional care and drive positive change in the care at home industry.”
Attendees can also learn about new solutions and practical applications of the insights shared during sessions by visiting an exhibit showcase featuring the latest products and services from leading care at home solution vendors. More than 50 organizations sponsored the 2024 AGILE conference.
Registration for AGILE 2025 will open in the fall of 2024. For more information, visit the AGILE conference website.
Axxess is the leading global technology innovator for healthcare at home, focused on solving the most complex industry challenges. Trusted by more than 9,000 organizations that serve more than 5 million patients worldwide, Axxess offers a complete suite of easy-to-use software solutions that empower home health, home care, hospice, and palliative providers to make healthcare at home human again. Multiple independent certifications have confirmed that Axxess has the most secure and industry-compliant software available for providers. The company’s collaborative culture focused on innovation and excellence is recognized nationally as a “Best Place to Work.”
©2024 Axxess All rights reserved
by Kristin Rowan | May 2, 2024 | Product Review
by Kristin Rowan, Editor
Revenue Cycle Management (RCM) addresses several pain points for care at home agencies: coding errors, timely reimbursement payments, and employee workload. Available as both full-service and SaaS products, RCM automation offers higher reimbursement rates, lower overhead costs, and overall better efficiency for your agency. Not having a RCM tool leaves your agency at higher risk for nonpayment, audits, and lengthy revenue cycles that impede your ability to manage your agency’s revenue.
Last week, I had the opportunity to talk with Michael Greenlee, Founder and CEO of HealthRev Partners. Hannah Vale, Chief Strategy Officer, joined him on the call. They told me about the HealthRev Partners’ launch of their new RCM tool, Velocity.
About HealthRev Partners
HealthRev Partners offers OASIS & POC Review and Coding assistance to home health, hospice, and palliative care agencies. The partnership program starts with an initial telephone conference, followed by a live review of documentation with an OASIS expert with recommendations for accuracy and compliance. Additionally, they have a precepting partnership program to enhance clinician performance and documentation practices. The RN guided program offers OASIS documentation review and correction sessions to ensure accurate and compliant documentation. Their solutions aim to maximize reimbursements with faster turnaround and higher accuracy.
HealthRev Partners Launches Velocity
On April 1, 2024, HealthRev Partners announced the launch of a new SaaS solution for Revenue Cycle Management, Velocity. HealthRev Partners designed Velocity to transform RCM for multi-site agencies. In addition to RCM, the tool offers operational insights for optimization and growth. Velocity focuses on real-time analytics and operational efficiency by centralizing data between locations. If you have an in-house RCM team, Velocity can be a stand-alone SaaS. However, if you need it, it can also be a full-service solution with outsourced coding and RCM experts on the Velocity team.
About Velocity
According to Michael Greenlee, many agencies lack tracking of their aging accounts receivable and the status of their claims. Without these, agencies can be leaving hundreds of thousands of dollars stuck in the revenue cycle without ever getting reimbursement from the claim. Velocity works with any existing EMR to pull data from coding and billing information. The built-in quality assurance (QA) solution is automated and customizable for charting and documentation. HealthRev Partners launched Velocity to help agencies overcome some of the pain points agencies have with RCM, billing, and coding.
Features
- Productivity and Accountability Reporting: Whether using Velocity as an outsourced solution or SaaS, instantly see time-stamped productivity reports, accuracy reports, and clinician QA scoring
- Ai powered tracking: All claims in the 61-90 day and over 90 day segments are brought into the system for tracking with a follow-up reminder for each claim, payment information, and reasons for nonpayment.
- Claims forecasting: Velocity shows the current financial status of the agency, and with enough data in the system, can provide revenue forecasts simply by entering a future date into the reporting system.
- Pre-built database: All charting codes are built into the system and are searchable by keyword or phrase to reduce coding errors and increase reimbursement rates
- Platform agnostic: For many agencies, switching to a different EMR system costs more than the sticker price on the solution. With Velocity, there is no loss of data because it holds previous EMR data when you switch.
- Advanced Funding: Partners with Velocity have access to their AR funds before claims are processed, with an immediate credit line of up to $100,000, or 80% of the agencies AR.
Differentiation
Whether you need a software solution for your in-house RCM team or are looking to outsource your billing and coding to a partner, choosing the right RCM team is essential for your success. With so many RCM companies available in the market, it can be difficult to choose the right one. To choose the right RCM partner, there are a few factors to consider:
How does the solution or company match with the mission and vision I have for my agency?
HealthRev Partners has an “aspiration to develop innovative solutions that create boundless opportunities for our clients to advance their mission.”
Does the solution have the right tools for my success?
The analytics tools in Velocity can by customized to each agency’s KPIs. Velocity offers a fully supported software solution, a SaaS solution, and everything in-between to provide each agency with the level of support they need to succeed. Clinician productivity reports calculate clinician reimbursement by month. This shows which of your clinicians needs additional training and which should be recognized for their achievements, which can help to decrease your turnover rates. Velocity will custom build additional dashboards and measurements, included in the cost of the software.
Is the software solution safe for my agency and my clients?
Velocity is a HIPAA secure platform and is undergoing SOC-2 certification to protect your organization and the privacy of your patients.
Does the software partner have my best interests in mind?
Have you ever talked to someone who is so passionate about what they do that their energy is contagious? That was my experience in talking with Michael Greenlee, CEO and Founder of HealthRev Partners. Our one-hour scheduled software review meeting turned into a two hour conversation about what Velocity is designed to achieve. We also talked about how much potential it has to help home health, hospice, and palliative care agencies to survive.
Greenlee’s goal for Velocity is to have 0 claims go past 90 days for any agency they work with. They train each of their team members to meet the needs of an individual customer before they touch the account. HealthRev Partners offers “white glove service” to make good agencies great and to help partners dominate their marketplace. Michael partners with agencies he believes in as much as he believes in his own company. “We’re passionate about securing success for home health, hospice, and palliative care agencies across the nation.”
Future Considerations
Michael, Hannah, and I talked at length about what might be possible with Velocity. (So much so that Hannah asked if I was available to attend their next planning meeting.) AI capabilities are evolving and maturing at a rapid rate. Generative AI will become the standard for software solutions in care at home in short order. Michael’s passion for elevating the efficiency and prosperity of his home health, hospice, and palliative care agency partners will undoubtedly lead to even more innovation. Hannah Vale offered, “Our goal is to further enhance the sophistication of the AI. We consistently heed client feedback to creatively address their evolving requirements.”
To book a demo with HealthRev Partners, click here.
# # #
 Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. Additionally, she has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. Additionally, she has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com








 Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. Additionally, she has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. Additionally, she has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or 

