Exclusive Inside Scoop: PocketRN and Assisting Hands
PocketRN and Assisting Hands® Home Care Announce a National Strategic Partnership to Test Medicare Dementia Care Model
Guiding an Improved Dementia Experience (GUIDE) Model, a CMMI Program, Aims to Increase Care Coordination, Support for Caregivers
WASHINGTON, DC, UNITED STATES, January 16, 2025. Today, PocketRN, a leader in virtual nursing, and Assisting Hands, a leading home care company, announced they will form a National Strategic Partnership to test the Centers for Medicare & Medicaid Services (CMS) alternative payment model designed to support people living with dementia and their caregivers. Under CMS’ Guiding an Improved Dementia Experience (GUIDE) Model, PocketRN will be one of almost 400 participants building Dementia Care Programs (DCPs) across the country, working to increase care coordination and improve access to services and supports, including respite care, for people living with dementia and their caregivers.
Partnership Foundation
Assisting Hands’ partnership with PocketRN is rooted in the fact that a significant portion of their client base has a dementia diagnosis. Their franchised locations nationwide provide daily care and respite care for caregivers in the homes of people living with dementia, making this alliance a strategic and logical decision.

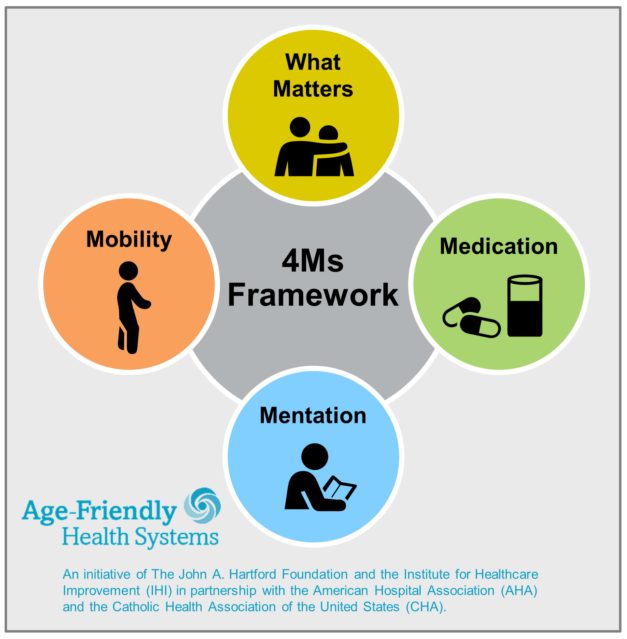
 Launched on July 1, 2024, the GUIDE Model will test a new payment approach for key supportive services furnished to people living with dementia, including: comprehensive, person-centered assessments and care plans; care coordination; 24/7 access to an interdisciplinary care team member or help line; and certain respite services to support caregivers. People with dementia and their caregivers will have the assistance and support of a Care Navigator to help them access clinical and non-clinical services such as meals and transportation through community-based organizations.
Launched on July 1, 2024, the GUIDE Model will test a new payment approach for key supportive services furnished to people living with dementia, including: comprehensive, person-centered assessments and care plans; care coordination; 24/7 access to an interdisciplinary care team member or help line; and certain respite services to support caregivers. People with dementia and their caregivers will have the assistance and support of a Care Navigator to help them access clinical and non-clinical services such as meals and transportation through community-based organizations.
PocketRN CEO
“We couldn’t be more thrilled to bring our revolutionary nurse-led care model to the millions of dementia patients and families who need it most,” said PocketRN CEO, Jenna Morgenstern-Gaines. “With PocketRN, patients and families get unwavering support from a ‘virtual nurse for life’ as they navigate the complexities of managing dementia at NO cost to them. Nurses are hands-down the best clinicians to be the ‘glue’ for patients and their families throughout their dementia journey–they’ve been doing so forever, and it’s high-time their work is valued by our system.”
“Assisting Hands is proud to announce our partnership with PocketRN. This collaboration reinforces our dedication to providing exceptional home care and respite services for individuals living with dementia and their caregivers. Together, we aim to enhance caregiver support and improve quality of life by offering comprehensive home care solutions and respite care, allowing caregivers to manage their responsibilities more effectively while ensuring their loved ones receive the best care possible.”
PocketRN Participation
PocketRN’s participation in the GUIDE Model will help people living with dementia and their caregivers have access to education and support, such as training programs on best practices for caring for a loved one living with dementia. The GUIDE Model also provides respite services for certain people, enabling caregivers to take temporary breaks from their caregiving responsibilities. Respite is being tested under the GUIDE Model to assess its effect on helping caregivers continue to care for their loved ones at home, preventing or delaying the need for facility care.
This model delivers on a promise in the Biden Administration’s Executive Order on Increasing Access to High-Quality Care and Supporting Caregivers and aligns with the National Plan to Address Alzheimer’s Disease. For more information on CMS’ GUIDE Model, please visit: https://www.cms.gov/priorities/innovation/innovation-models/guide.
# # #
About Assisting Hands® Home Care
Assisting Hands is a leading provider of in-home care services for seniors, individuals with disabilities, and those recovering from illness or injury. With over a decade of experience, Assisting Hands provides high-quality care in the comfort of the home, offering a range of services including personal care, companion care, and respite care. The company’s franchise system has grown rapidly, with locations across the United States.
About PocketRN
PocketRN gives patients, families, and caregivers a “virtual nurse for life.” Its mission is to close the gap between home and healthcare by: enabling nurses to care proactively and continuously at the top of their license, enabling caregivers with peace of mind and the confidence to support others, and enabling patients to access whole-person, trusted, empathetic care when and where they want it. PocketRN is the glue that holds together fragmented experiences in care so that partners, clinicians, patients, and families get back more of what they need: quality time. For more information, visit www.pocketrn.com
This press release will appear on EIN Presswire and was submitted to The Rowan Report as an exlusive advanced release, printed with permission.