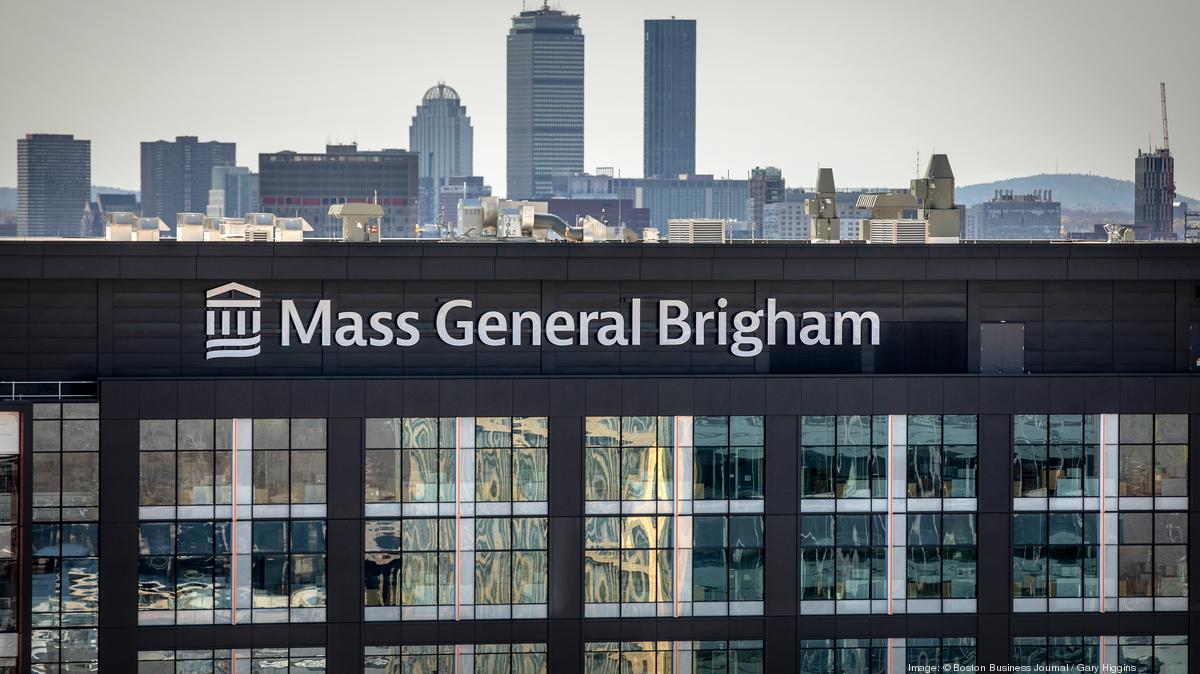
Patient Relationships Drive Satisfaction
by Kristin Rowan, Editor
Caregiver Motivation
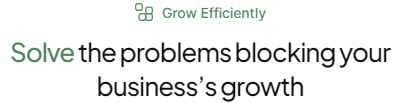
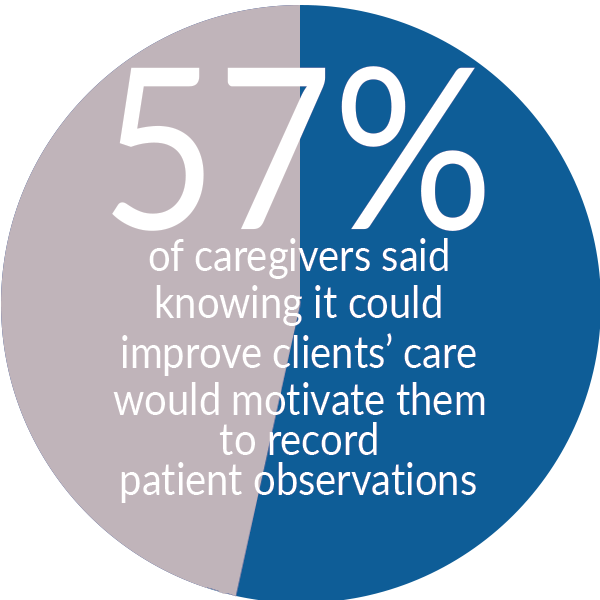
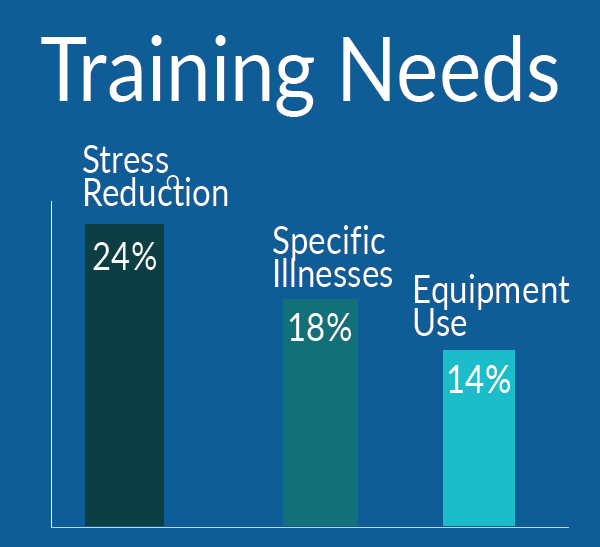
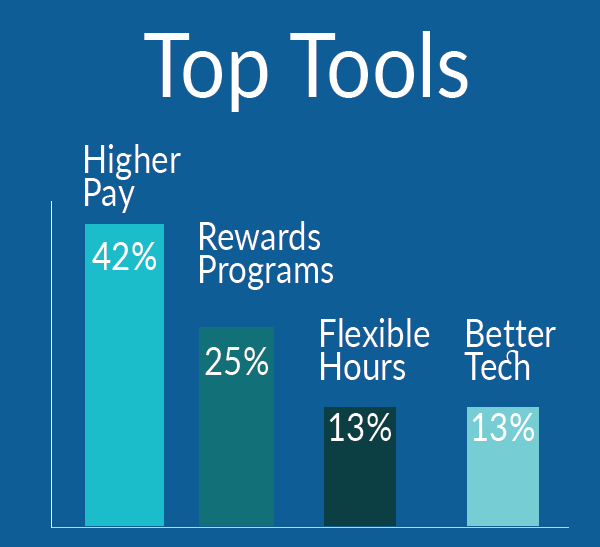
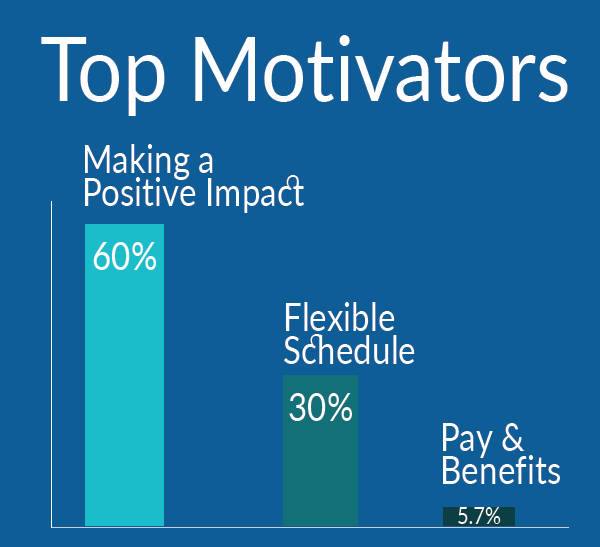
HHAeXchange recently conducted a survey of more than 3,900 caregivers. The company set out to understand caregiver motivation and to use this information to increase caregiver satisfaction and improve outcomes.
Highlights
This data highlights the motivations of caregivers to improving health and wellness for their patients
From HHAeXchange
While the challenges and demands of being a caregiver still remain – low compensation, feelings of stress and exhaustion, and risk of catching infectious diseases – this survey shows that caregivers remain committed to their work to improve the lives of their patients. As more individuals seek homecare options, the homecare industry must continue to evolve to ensure caregivers are given the resources and recognition they need to remain motivated and focused on patient care.
For more details and information about the study, see the HHAeXchange press release.


Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com