Industry Update
Adminby Kristin Rowan, Editor
Industry Update with Dr. Steve Landers
At last week’s New England Home Care & Hospice Conference, Dr. Steve Landers, President of The National Alliance for Care at Home (The Alliance) gave the keynote address and offered some industry insights and updates.
A Heartfelt Introduction
Ken Albert, Chairman of the Board at The Alliance introduced Dr. Landers before his address. After reading Dr. Landers’s official biography, Albert offered his own thoughts on the first few months of Landers’ tenure.
Last year, five colleagues from organizations across the country sat in D.C. interviewing candidates. While interviewing Landers, I was remarkably engaged by someone who is deeply passionate about care at home. Steve describes hospice care as a national treasure, and I don’t disagree. More than just his passion for care at home, Dr. Landers is savvy in navigating the political paradigms driving policy. He artfully combines data and stories to navigate relationships with policy makers. What I see every day is someone who roles up his sleeves for the patients we take care of with tremendous respect for the caregivers who are in the patients’ homes.
Industry Changes, Advancements, and Ongoing Advocacy Efforts
Dr. Landers attributes much of the positive changes in D.C. to the efforts of volunteer leaders looking to move the industry forward. Care at home needs to become more streamlined, more efficient, and with a better voice.
His vision for the care at home industry is an America where everyone can access high-quality care wherever they call home.
Strong Admonition for CMS
Dr. Landers noted positive movement in some areas. However, he became passionately adamant that a payment update is not an increase if it doesn’t keep up with inflation or pay increases. “The Alliance represents providers delivering high-quality, person-centered care to million of individuals in the home, and they deserve to be recognized and compensated for the work they do,” he said.
Our Aging Nation
It should come as no surprise that older adults have a strong preference for aging at home. They prioritize living where they feel in control and connected. They want to be in familiar surroundings and to maintain their routines.
The U.S. population over the age of 85 is expected to triple from 2020-2060 to more than 19 million people. Despite medical advances, only 1/3 of those over the age of 85 say they are free of disability or free of difficulty with daily living.
With the rising number of older individuals, caregiver to patient ratios are falling nearly everywhere across the country. Dr. Landers and The Alliance urge policymakers to make promoting the dignity and independence of our aging population one of their highest health policy priorities. The Alliance will continue to tell anyone and everyone who will listen that care at home offers the win-win solution that policymakers are looking for.
Changes at the Top
We’ve already seen numerous and sometimes drastic changes at the federal level. Dr. Landers points out that eight years ago the “Trump 1.0 Administration” developed the PDGM framework and signed hospice reform legislation. On the campaign trail, President Trump stated he would not be making cuts to Medicare. The “Trump 2.0” care at home priorities are not yet clear, but The Alliance will continue to emphasize cost savings and the preference to age in place.
Secretary Kennedy, head of HHS, placed his emphasis on the chronic disease epidemic, launching Making America Healthy Again. He has stated a preference for community-based solutions and patient-centered care.
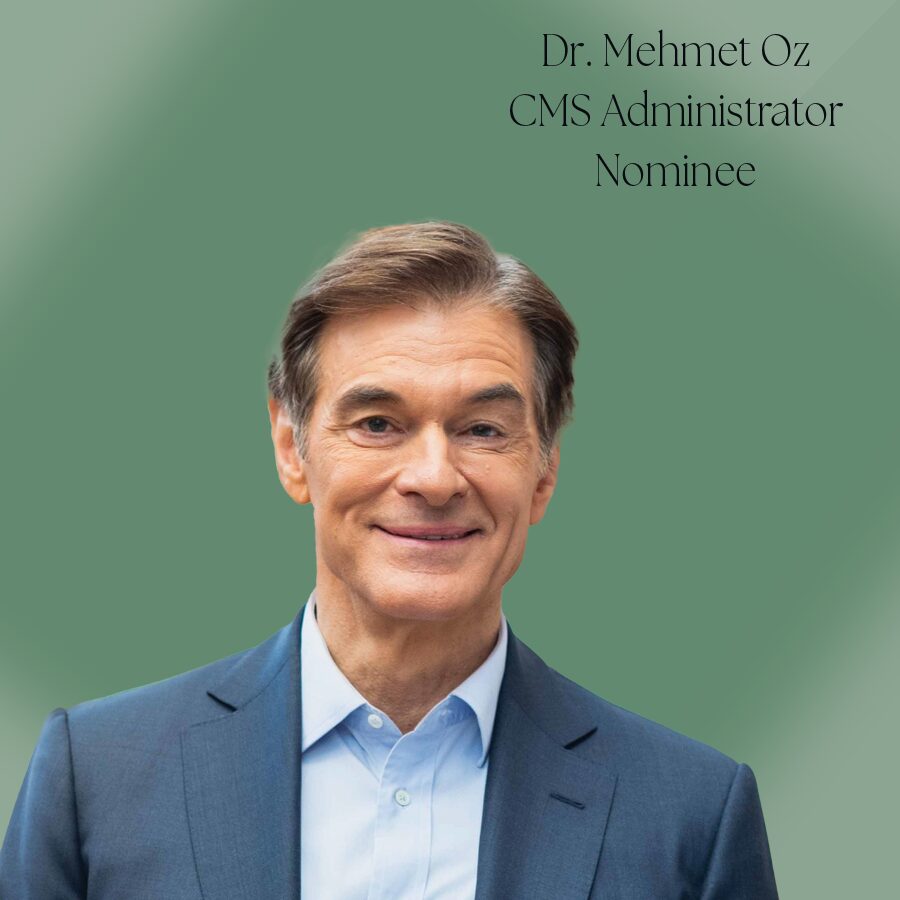
New CMS Administrator Dr. Oz seems to be supportive of Medicare Advantage, but did have some critique of the program during senate hearings. Dr. Oz has a stated focus of finding and eliminating fraud, waste, and abuse.
Changes Near the Top
At the congressional level, The Alliance lost a few key supporters with the last election, but many care at home advocates remained. Of the returning members of the Senate and House, care at home advocates include:
- Senators Collins (R-ME), Hassan (D-NH), Tillis (R-NC), Barrasso (R-WY), Blackburn (R-TN), CortezMasto (D-NV), and Rosen (D-NV)
- Representatives: Adrian Smith (R-NE), Sewell (D-AL) Van Duyne (R-TX), Panetta (D-CA), Guthrie (RKY), and Carter (R-GA)
The support in Congress leaves us hopeful. Large Reconciliation Packages dominate the current conversation. Many questions remain as to what is at risk for care at home and what Medicaid’s future might hold.
Later this year, The Alliance sees opportunities for care at home outside of reconciliation. These include Home Health PDGM reform, hospice reform, the telehealth extension, revocation of the Medicaid HCBS 80/20 rule, tax credits, and long term care insurance.
Public Policy Priorities
As The Alliance moves forward, several key issues will remain priorities:
Access to Care at Home
- PDGM Implementation
- Telehealth Extension
- Medicare Advantage Dynamics
- Care for High Needs Beneficiaries
Quality Care at Home
- Special Focus Program Implementation
- DEA Telehealth Provisions
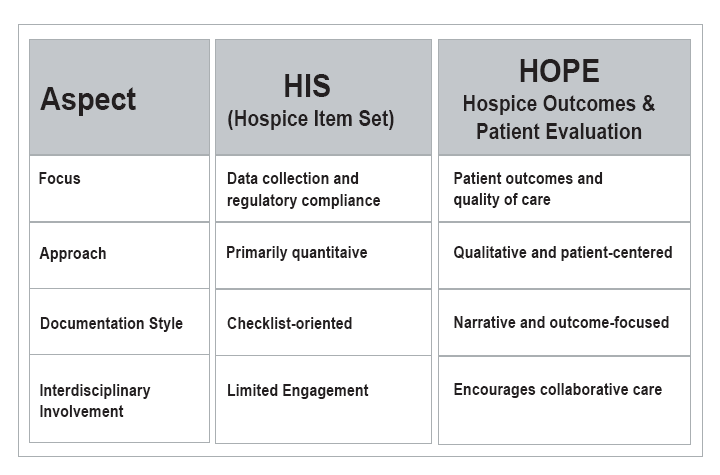
- HOPE tool implementation?
Eliminating Fraud and Abuse in Care at Home
- Hospice Concurrent Care
- Hospice and Medicare Advantage
- Medicaid 80/20 Rule
- Caregiver Tax Credits / LTCI
Growing the Care at Home Workforce
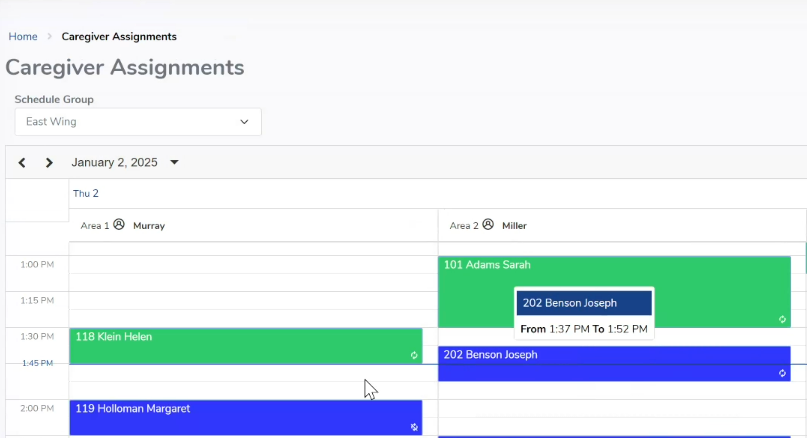
- Supply is simply not meeting demand
- Strengthened rates, incentives, and educational opportunities will attract and retain a qualified workforce
Follow Up
I spoke with Dr. Landers after the keynote address to ask him why lone worker safety was not among the top priorities of The Alliance. He assured me that there is a position within The Alliance who, among other tasks, is focusing on lone worker safety. I urged him to make it a higher priority and will follow up to get the contact information for the position he mentioned.
# # #


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com