Groped by Patients
Adminby Elizabeth E. Hogue, Esq.
Groped by Patients
Just a Slap on the Wrist
Many aides in a variety of healthcare settings have been the victims of unwanted touching or groping. What should they do? In Dorothy Bills v. WVNH Emp, LLC, and Lanette Kuhnash [No. 2:22-cv-00093 (S.D.W. Va., 2022)], the Court concluded that slapping the hands of groping patients is inappropriate conduct.
In this case, a Certified Nursing Assistant (CNA), Dorothy Bills, was responsible for the care of a patient who had limited mental capacity. He could not control his actions or understand their effect. He was sexually aggressive, and staff members had already been instructed to care for him in pairs.
Dorothy Strikes Back
Dorothy Bills was in the patient’s room alone while another nurse was on her break. She moved close to the patient’s bed to speak to him because he was hard of hearing. The CNA leaned closer to the patient to provide water and to help him stay in bed as he tried to sit up. As she did so, the patient reached out and touched Ms. Bills’ breast and vaginal area. He touched her inappropriately on multiple occasions when she cared for him, so she smacked his hands in response and told him that it wasn’t nice to touch her.
A coworker told Ms. Bills that slapping the patient’s hands was abuse and she must report the incident.
Agency Policy
The provider, WVNH, had a policy that prohibited physical abuse, including any form of corporal punishment defined as physical punishment used as a means to correct or control the patient’s behavior. The policy specifically prohibited slapping patients’ hands.
Rapid Escalation
The CNA filed an incident report that said she smacked the Patient’s hands three times. She said she didn’t slap him hard enough to hurt him, but just as one would a child who was misbehaving. As a result, a report was made to adult protective services and Ms. Bills was suspended. Adult protective services dropped the allegation of neglect. The CNA’s employment was terminated and her license later expired.
Groped by Patients, and the Court
Ms. Bills filed suit several years later on the basis that her termination was wrongful because it was in retaliation for resisting sexual harassment. She described slapping the patient’s hands and scolding him to “reprimand” him “like you would a child misbehaving” in both the incident report she filed and during her deposition. Consequently, the Court said that the only issue is whether employers are prohibited from firing employees who physically punish a patient in response to sexual harassment.
The Court concluded that smacking patients’ hands and scolding them are inappropriate activities. Physically punishing patients, said the Court, is not a reasonable means of opposing sexual harassment by them. Filing complaints and asking for protective measures is appropriate. The CNA appealed the Court’s decision to the United States Court of Appeals for the Fourth Circuit. On April 29, 2024, the appeals court issued a decision upholding the lower Court’s opinion.
Prevention as a Cure for Being Groped by Patients

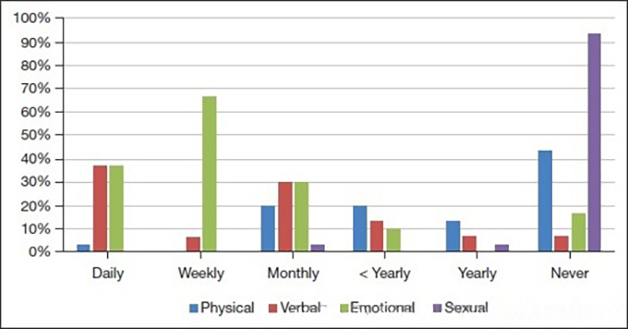
Here are some practical actions that may help prevent sexual harassment of staff members by patients:
- Providers should require staff members to document and report every instance of sexual harassment by patients.
- Staff members who violate the policy should be disciplined.
- Patients should be evaluated by appropriate clinical staff to determine whether medication may be helpful to address inappropriate touching.
- Staff members should receive education and training on a regular basis about the causes of inappropriate touching and how to address it.
Final Thoughts
The bottom line is that sexual harassment is not a part of the job description of staff members and providers must take appropriate steps to protect them.
# # #


Elizabeth Hogue is an attorney in private practice with extensive experience in health care. She represents clients across the U.S., including professional associations, managed care providers, hospitals, long-term care facilities, home health agencies, durable medical equipment companies, and hospices.
©2025 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com