Planned Parenthood Cut Halted
CMSby Kristin Rowan, Editor
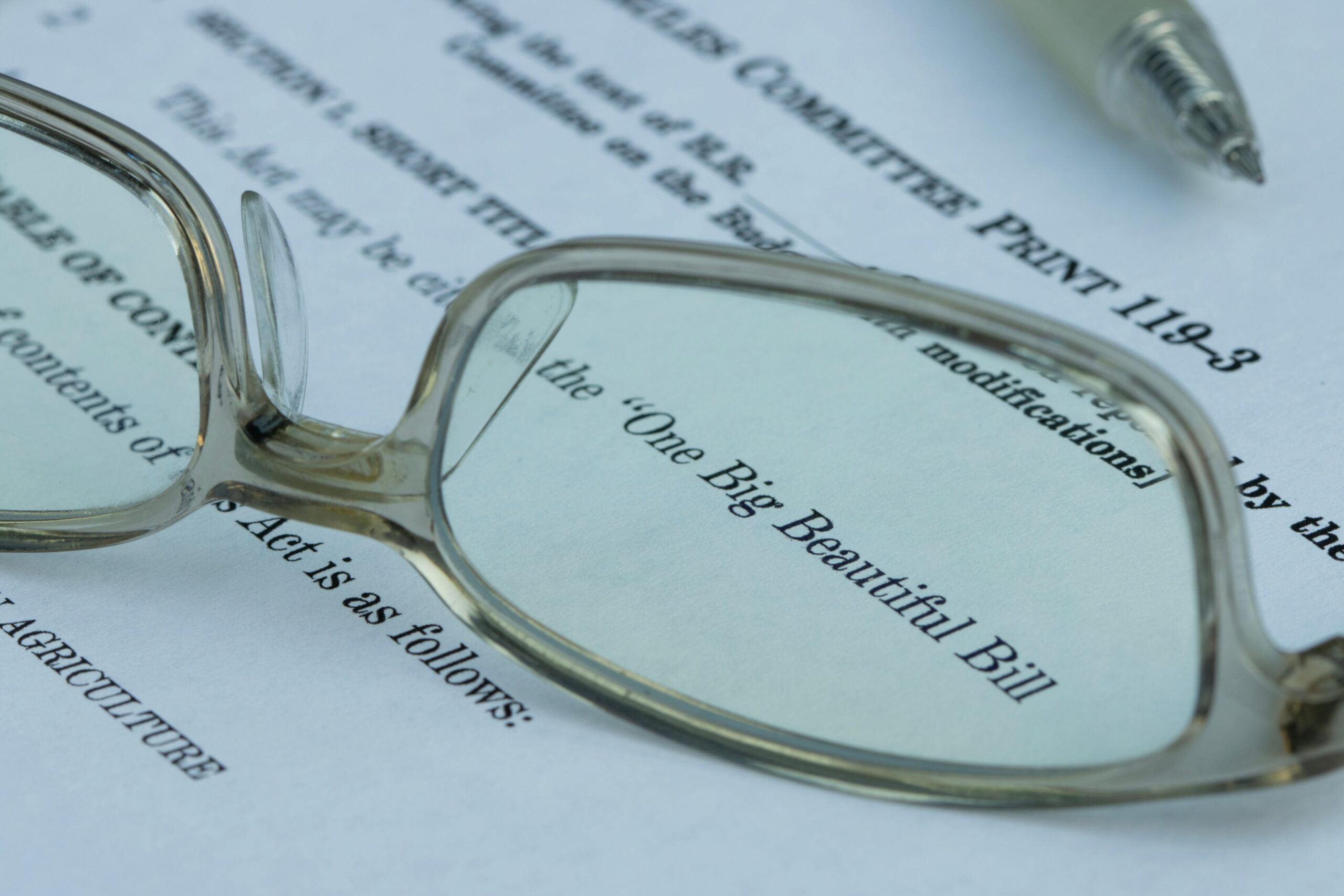
Part of Big Beautiful Bill Halted
Medicaid Cuts to Planned Parenthood Blocked
The tax and immigration bill, dubbed “One Big Beautiful Bill,” signed by President Trump on July 4th, included removing all Medicaid payments to any nonprofit organization that provides medical services, received more than $800,000 in federal funding in 2023, and also provides abortions.
On Monday, July 7th, the first business day after the bill was signed into law, U.S. District Judge Indira Talwani granted a temporary halt to Medicaid funding cuts to Planned Parenthood.
Planned Parenthood Claims Unfavorable Treatment
The portion of the bill in question does not specifically name Planned Parenthood. The bill cuts Medicaid funding to groups “primarily engaged in family planning services, reproductive health, and related medical care” that also provide abortions and abortion education. According to the lawsuit, however, because of the federal funding threshold of $800,000, Planned Parentood locations comprise almost all of the impact.
[It’s a] “naked attempt to leverage the government’s spending power to attack and penalize Planned Parenthood and impermissibly single it out for unfavorable treatment.”
Immediate Decision
The decision came before the federal government responded. Judge Talwani ruled within hours and provided no explanation other than a brief note stating that Planned Parenthood showed good cause for immediate intervention.
Decision Unlikely to Stand
- The decision came within hours of the lawsuit filing
- Congress is generally lawfully allowed to make determinations on spending
- This was an egregious judicial usurpation of legislative power
- This makes her court look like a fast food drive-through
- The House could initiate impeachment proceedings against the judge for this decision
These are just a few of the statements made in opposition to the injunction, mostly claiming that the judge did not have the authority to make the decision. Talwani set a hearing for July 21 to hear from both Planned Parenthood and the agencies named in the lawsuit, HHS, and CMS.
Precedent
A previous ruling from the Supreme Court in June of this year provides that any state can remove any provider from the list of “Qualified Providers” using its own Medicaid criteria. The court further ruled that, although patients have the right to choose their own provider, patients do not have the right to sue based on who those qualified providers are.
This lawsuit is the first against the tax and immigration bill, but it is most likely not the last. We will continue to report on this and other lawsuits as they arise.
# # #


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com