Creditable Coverage for Medicare Part D
Adminby Kristin Rowan, Editor
CMS 2026 Updates to Prescription Plan
The Centers for Medicare & Medicaid Services (CMS), as part of the Inflation Reduction Act of 2022 (IRA), released a draft of the calendar year 2026 redesign program instructions. The new provisions for Medicare Part D include:
- An annual out-of-pocket maximum of $2,100, up from $2,000 in 2025
- A selected drug subsidy program
- The requirement that Part D plans offer enrollees the option to spread out their out-of-pocket costs over the year
- Maximum charge of $35 for insulin regardless of deductible, co-pay, or out-of-pocket spending reached
- No out-of-pocket costs for recommended vaccines
- New requirements for Creditable Coverage
Current Creditable Coverage Determination
The current simplified determinations method is as follows:
- The plan provides coverage for brand and generic prescriptions;
- The plan provides reasonable access to retail providers;
- The plan is designed to pay on average at least 60% of participants’ prescription drug expenses; and
- The plan satisfies at least one of the following:
- The coverage has no annual benefit maximum or maximum annual benefit payable by the plan of at least $25,000;
- The coverage has an actuarial expectation that the amount payable by the plan will be at least $2,000 annually per Medicare-eligible individual; or
- For employer plan sponsors that have integrated prescription drug and health coverage, the integrated plan has no more than a $250 deductible per year, has no annual benefit maximum or a maximum annual benefit of at least $25,000, and has no less than a $1,000,000 lifetime combined benefit maximum.
Creditable Coverage
Medicare beneficiaries must enroll in Medicare Part D, unless they have other prescription coverage. If a beneficiary goes more than 63 days without prescription coverage, they may incur a late enrollment penalty. Creditable coverage has to have a value equal to or greater than the defined coverage for Part D. This requirement is not new. Group health plans have been calculating creditable coverage since the inception of the Part D program. What is new is that CMS has determined that the simplified method of determining creditable coverage is no longer accurate. The revised method must include all of the following:
- Provide reasonable coverage for brand name and generic prescription drugs and biological products
- Provide reasonable access to retail pharmacies
- Is designed to pay on average at least 72% of participants’ prescription drug expenses
Impact
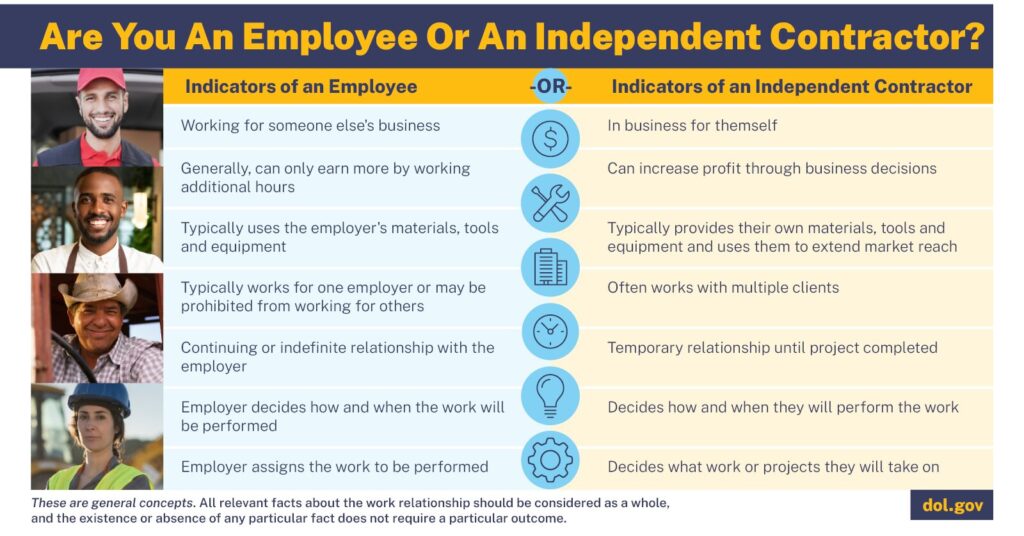
Persons over the age of 65 who qualify for Medicare, but who are still employed may have an employer sponsored or paid health insurance plan. Many of these plans have combined health and drug coverage. These plans will now have to provide creditable coverage, presumably for all beneficiaries, not just those who are eligible for Medicare.
- The coverage has no annual benefit maximum or maximum annual benefit payable by the plan of at least $25,000;
- The coverage has an actuarial expectation that the amount payable by the plan will be at least $2,000 annually per Medicare-eligible individual; or
- For employer plan sponsors that have integrated prescription drug and health coverage, the integrated plan has no more than a $250 deductible per year, has no annual benefit maximum or a maximum annual benefit of at least $25,000, and has no less than a $1,000,000 lifetime combined benefit maximum.
For Additional Information
If you are currently offering an employee sponsored health plan, or need more information on Part D coverage, refer to the CMS Fact Sheet and the Program Instructions.
# # #


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news .She also has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com