by Kristin Rowan | Oct 25, 2024 | Admin, Advocacy, Regulatory
Dr. Steven Landers brings his almost 20 years of experience to The Alliance as its first CEO. Dr. Landers is a board-certified physician in family medicine, geriatric medicine, and hospice and palliative medicine. He has dedicated his career to seeking home- and community-based solution to traditional healthcare. His focus is on providing compassionate, dignified, and cost-effective care to patients.
Dr. Landers graduated from Case Western Reserve University School of Medicine, where he completed a geriatric medicine fellowship at the Cleveland Clinic.
Dr. Landers is no stranger to NAHC and NHPCO, having previously served on the board of directors for NAHC. He has met with Congress, state legislatures, CMS, and PAC officials, providing testimonies, discussing home care policy and regulation, and advocating for care at home.
Steve lives in Little Silver, New Jersey, with his wife, Allison, and their three sons. His hobbies include golfing, fishing, hiking, traveling, enjoying good food and watching horse racing. When he is not taking part in these activities, you can find him cheering on his sports teams — the Browns, Cavaliers, Guardians and Indiana Hoosiers.
Dr. Steven Landers: On the Record
The Rowan Report:
What do you know about the status of the ongoing lawsuits, going back to the 2024 final rule?
Dr. Steven Landers:
One, we should probably bring Bill [Dombi] into it because he’s truly a technical expert on it and I’m still getting up to speed on it. My understanding is there is no active lawsuit at the moment. We were asked to go back and take some additional administrative steps, which we’re doing. Then we’ll be able to evaluate what further legal paths are possible.
RR:
That leads me to, not a question, but an observation I’d like you to comment on, Steve. For 45 years, the organization has been run by attorneys and the emphasis in lobbying and advocacy has been ‘you need to stop this cut because it’s hurting businesses and also it’s hurting patients.’ The way you’re talking, you emphasize as you begin with how it’s hurting patients. And so I’m wondering if the organization being run by a physician and not an attorney indicates that different emphasis going forward.
Steve:
I certainly am going to do everything I can to tell the story of how policies impact patients and families. That will be part of what I try to do every single day using my experiences as a physician to do that.
RR:
Would it be exaggerating to say “new day, new emphasis” at The Alliance?
Steve:
Well, The Alliance is new in and of itself, so The Alliance is a new day for the industry, a hundred percent. We brought together two legacy organizations. The opportunity to have a stronger voice is very real and certainly I am going to bring a clinical perspective. I’m also a family caregiver. I have my own personal experiences with home care and hospice that have instructed how I think about these things.
And there is every opportunity here to get stronger, to try to make a bigger impact. I would not diminish the truly heroic work that’s been done by advocates within our associations in the past. There’s a lot of love and care that’s happening out in our country because of the leadership that’s been in place. But as you can see by some of the things that we’re talking about, we need to do better. We need to find another way to tell these stories to somehow get somebody to listen.
RR:
You recently released a statement about your position as CEO of The Alliance and your vision going forward. There was a commitment attached to that. Can you speak to that?
Steve:
Yeah, so that’s one of the things that I’m really happy we’re doing very early in our work with the Alliance. For membership, whether to join or to renew membership, we are requiring an attestation from our members around their commitment to quality and to compliance. We’re requiring any provider member to attest to having a program in place for quality and compliance. And we’re requiring that they attest that they monitor the OIG exclusion list and don’t take referrals for employees that are people that are on that list. Also for home health and hospice providers, we’re asking that they attest that they do their level best to participate in the Medicare Home Health and the Medicare Hospice Quality Reporting program.
In order to make a difference on behalf of our members and make a difference on behalf of the people that need care at home, we have to have as credible and high integrity of a voice as possible. And so this is just one simple step of additional things that we’ll consider going forward. We want to make sure that our alliance, our coalition is high integrity and has a deep commitment to quality and compliance.
RR:
It’s one thing to ask people to sign an attestation. It’s another to find the bad players and help CMS to get rid of them.
Steve:
And we’re right there as a partner in that. I think you’ll see more announcements from us in the future about what we’re doing to help with that. I mean, on one hand, we’ve made many proposals around fighting fraud and hospice in particular. If you followed the hospice policymaking, both Legacy NAHC and Legacy NHPCO over the last year have made many policy recommendations. And you’ll definitely see us both advocating for anti-fraud measures as well as having resources within our association to focus on those topics.
Interviewer 1:
Just to clarify, did either of the legacy organizations have this same kind of attestation?
Steve:
No, this is new. The impact of the legacy organizations cannot be questioned. It’s been amazing. But, it’s a new day and we are looking at ways to increase our impact. So, this is a new part of our membership process that we feel strongly about to just take another step to ensure that our coalition, our membership, is of the highest integrity possible. We are walking the walk and talking the talk with respect to quality and compliance.
RR:
Thank you, Dr. Landers
This article is part 1 of 2 interviewing Dr. Steven Landers. Read the rest of the interview here.
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Kristin Rowan | Oct 10, 2024 | Clinical, Regulatory
Elderly Patient Needs 24-hour Care
In Polk County, FL, an 86-year old man, identified only as Mr. Anderson, was hopsitalized and diagnosed with congestive heart failure. In addition to receiving care from Good Shepherd Hospice, his family hired round-the-clock care through Assisting Hands. The home health aides were caring for Mr. Anderson in 12-hour shifts.
Beatrice Taylor arrived for her night shift at 9 p.m. She noted that Mr. Anderson and his wife were already in bed, but not sleeping. Shortly after the day aide left, Taylor fell asleep on the couch in the living room of the patient’s home. Company policy states she was responsible for the patient’s care and should not have been sleeping.
Taylor was awakened by a “thump” coming from the bedroom. She entered the bedroom to investigate and found Mr. Anderson lying on his side, on the floor, with his head wedged between the nightstand and the bed. Taylor told investigators that she tried to help him back into the bed. He told her not to touch him, so she left him there and went back to sleep on the couch. She did not call 911, as was the policy of Assisting Hands in the event of an emergency. Nor did she call her agency or anyone else to assist.
Taylor woke up somewhere between 3:45 a.m. and 4:53 a.m. that morning. At some point, she called her parents and had a 36 minute conversation. During that conversation, she decided to check on the patient and found him still on the floor, but now unresponsive. It was her parents who suggested she call 911.
Contrary to both her parents’ urging and her employer’s policy, Taylor still did not call 911. Instead, she called Assisting Hands and left a message through the company portal. Taylor finally called 911 at 5:37 a.m., more than four and a half hours after Mr. Anderson fell.
The implanted pacemaker found during autopsy showed that Mr. Anderson was still allive at 1:oo a.m. when Taylor initially found him. The autopsy also concluded that he would have survived if Taylor had called 911 right away. His official cause of death was positional asphyxia with pre-existing health conditions listed as contributory causes.
Not actual image from story
During the course of their investigation, detectives reviewed the Assisting Hands employee policies. That investigation uncovered several policies that Taylor violated:
- If a patient falls, home aides are required to seek help which may entail calling 9-1-1. Home aides must notify the company as soon as the patient is safe
- Home aides are not permitted to sleep during their assigned shift unless it is a “live in” shift
- Home aides are required to submit care notes using the company portal throughout their shift to ensure assigned services are being followed appropriately.
The 911 call that Taylor placed at 5:37 a.m. should have been placed at 1:00 a.m.
Assisting Hands confirmed to detectives that this was not a “live in” shift
No information was provided as to whether Taylor submitted care notes during the shift.
Taylor worked for Assisting Hands for eight months, but did not show up for her shift following the incident with Mr. Anderson. Assisting Hands has since terminated her employment. She was a licensed home health aide, but does not have a medical license, nor is she a nurse.
Taylor was arrested by detectives and made several statements about her innocence. She insisted she had done nothing wrong saying she, “didn’t kill that man.” A paramedic who responded to her 911 call overheard Taylor on the phone say, “he was old anyway so what does it matter.” Taylor remains in custody at the Polk County Jail and is being held without bond.
“The complete disregard for Mr. Anderson’s life by the person who was employed by his family is completely outrageous, and egregious. I believe someone who was not even being paid to look after this elderly man would have immediately dialed 9-1-1 under these circumstances. Her behavior and attitude are simply deplorable. Mr. Anderson’s family members are in our prayers.”
Sheriff, Polk County Sheriff's Office
In 2021, more than 38,000 older adults died from falls. This is the leading cause of injury death for adults aged 65 and older. The death rate increased 41% between 2012 and 2021. You can read more about the risk of falling and what one company is doing to help prevent falls in our accompanying article this week, an interview with Dr. Ann Wells of InnovAge.
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Rowan Report | Aug 9, 2024 | Admin, Caring for the Caregiver, Clinical
This article is part two of a two-part series. You can read part one here.
by Todd Austin and Sasha Erickson
3 Steps Towards Creating a Culture of Love that Retains Employees
In a study done on the “Culture of Companionate Love and Employee and Client Outcomes in a Long-Term Care Setting,” researchers found displaying warmth, affection, and connection had a tangible impact on employee turnover, resident outcomes, and family satisfaction.
Employees who felt they worked in a loving, caring work environment reported higher levels of satisfaction, increased teamwork, and showed up to work more regularly. But the effects of a companionate culture aren’t just felt by your employees.
Research shows that employees who work in a culture of love companionate culture directly related to client outcomes such as improved patient mood, quality of life, satisfaction, and fewer trips to the ER.
A culture like this is only made possible through a conscious effort from leadership to make their employees feel cared for and appreciated. To see similar results in your own business, start creating a culture of love.
Be an advocate for your employees' mental health
Contrary to popular opinion, an employee doesn’t leave their emotions at the door when they come into work. Especially if they work in a service-based industry like long-term and post-acute care.
The emotions an employee feels while caring on the job affects performance, customer and employee satisfaction, and care outcomes.
For example, if an employee is feeling stressed, frustrated, or disgruntled, they will either appear so as they’re caring for their residents and patients or be forced to put up a positive front on the outside while bottling up negative emotions on the inside. Whether these types of negative emotions are revealed in the open or held within, either outcome leads to low satisfaction and high employee turnover.
Instead, be an advocate for your employees’ wellbeing and mental health. Provide resources for mental health support and regularly check-in with your staff at important milestones. Offering competitive benefits, flexible hours, and paid time off encourages employees to tend to their own needs as well as others.
Broaden your company’s definition of culture
Culture is more than a staff break room with a foosball table. Your company’s culture will create itself, whether you’re in control of it or not.
Creating a healthy company culture requires deliberate and consistent actions from your leadership team. It is your goal to ensure that when your employees think about work on a Sunday night, they feel positive about coming to work every Monday morning. At Activated Insights, our approach centers on understanding and enhancing the employee experience through several key strategies:
-
-
Culture and Engagement Assessments
- We regularly administer assessments to identify strengths and areas needing improvement to help us stay attuned to the evolving needs and perceptions of our employees.
-
Employee Focus Groups and Culture Audits
- We have started administering focus groups and culture audits to gain real insights and solutions directly from our employees. These sessions create open lines of communication where employees can express their thoughts and ideas.
-
Prioritizing Employee Wellness
- We offer unlimited PTO with mandatory minimums, including one mental health day off each quarter and a minimum of two weeks off per year with at least one period of five consecutive days off. This policy underscores our commitment to employee well-being, ensuring that they can balance work with personal life effectively.
-
Effective Communication and Leadership
- Continuously communicating, modeling, and reinforcing the company’s vision, values, mission, and guiding principles is crucial. Leaders play a significant role in setting the tone and maintaining a positive culture by leading with transparency, empathy, and consistency.
-
Team Building and Collaboration
- At Activated Insights our teams are often comprised of both in-office and remote employees. We encourage teams to get together at least annually. It’s imperative that companies are deliberate in providing opportunities for their teams to collaborate, build trust, and break down silos. We find that this improves overall job satisfaction and productivity.
-
Building Trust and Accountability
- Trusting employees and treating them like adults to manage their work and personal demands is essential. By creating an environment of trust and accountability, we encourage employees to take ownership of their roles and contribute meaningfully to the organization’s success.
By focusing on these strategies, we ensure that our employees look forward to coming to work, feel valued and supported, and are motivated to contribute to a positive company culture.
Learn to speak your employees’ professional “love language”
If you don’t speak two languages, you won’t connect with your employees to make them want to stay.
While everyone communicates in their own way, if you don’t know the language your caregivers will listen to, your recognition efforts are going to waste.
But this isn’t the type of language Duolingo can teach you. Rather, every provider in the long-term and post-acute care industry should become fluent in appreciating their employees.
The Value of Communication
In 1992, Dr. Gary Chapman noticed a pattern of miscommunication after practicing couples’ counselling for years. He discovered that individuals often misunderstand one another’s needs by communicating how they would personally like to receive recognition, without taking the others’ needs into consideration. He concluded that how we respond to appreciation boils down to one of the following categories.
Learn how to speak your caregivers’ language of appreciation to increase caregiver retention, refine your leadership skills, and foster a culture of recognition:
Professional Love Languages
- Words of Affirmation
- Care employees ranked verbal recognition by a supervisor as their number one preferred form of recognition—and lack of communication from their employer as their top complaint. Actively seek out reasons you can praise your caregivers to boost company morale and foster a culture of gratitude:
- Send handwritten thank you cards
- Give your caregivers a shoutout in company newsletters or on social media
- Recognize top performers using an employee of the month program to give everyone a chance to be in the spotlight
-
Receiving Gifts
- While a raise may be outside of the company budget, 20.4% of caregivers mentioned smaller forms of monetary recognition as their chosen form of acknowledgement. Small bonuses for top performers, extra vacation time, or gift cards are simple forms of appreciation:
- Give gift cards or free movie tickets
- Give company branded clothing
- Offer paid vacation time
-
Acts of Service
- A care employee’s occupation is to literally provide service to those in need—but have you ever thought of ways to serve your care staff? Although it may seem counterintuitive to serve in a workplace where employees are paid, you can offer your staff the relief that they need by helping to shoulder some of their responsibilities:
- Gather feedback and listen to how you can make their daily tasks or commute a little easier
- Go the extra mile to make them smile by hosting random appreciation events where you can offer the company donuts, coffee, or even turkeys on Thanksgiving
- Quality Time: Caregiving can be a very isolating job where they receive little social interaction with people other than their clients. Consciously create opportunities to spend quality time with your caregivers:
-
- Hold group training events to create an environment where caregivers can ask questions and learn from fellow coworkers.
- Schedule one-on-one meetings or lunches to build individual relationships with your caregivers and check in on how they are doing.
- Support their learning and professional development by discussing your caregivers’ goals and needs
So, What Does Love Have to Do With It?
In short: everything.
Your ability to create a companionate culture of recognition for your care staff will be the difference that pulls you out of the revolving doors of recruitment and retention.
The quality of your leadership within your company directly impacts your quality of care for the long-term and post-acute care industry.
In 2024, spend more time consciously creating a companionate culture and start to see your employee retention and client satisfaction skyrocket.
As a highly accomplished executive, Todd Austin, COO & President of Activated Insights, is recognized as a leading voice in the rapidly-growing care industry. With over a decade of experience in executive leadership roles, Todd brings a wealth of knowledge and expertise to his current position as a key member of the Activated Insights team.
With a background in sales, marketing, management, operations, and finance, Todd is a true Renaissance executive with a rare combination of strategic and tactical skills. His expertise in developing and implementing growth strategies, optimizing operations, and driving profitability has made him a sought-after advisor to many organizations.
Sasha Erickson is the Director of Talent at Activated Insights, formerly HCP. With over 10 years of experience in human resources across a variety of industries, Sasha has worked with organizations ranging from small businesses to Fortune 500 companies. She graduated Summa Cum Laude from Utah State University with a degree in Business Administration and minors in Human Resource Management, Marketing, and Finance.
Sasha’s career history includes roles at Avant Guard Monitoring Centers, Goldman Sachs, Schreiber Foods, JBS and Pilgrim’s Pride Corporation, RR Donnelley, and Denver Public Schools. Her expertise spans talent acquisition, employee engagement, culture development, HCM software implementation, and strategic HR management.
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Rowan Report | Aug 1, 2024 | Admin, Caring for the Caregiver, Clinical
This article is part one of a two-part series from Activated Insights, formerly Home Care Pulse. Come back next week for the continuing story. Read more about Caring for the Caregiver here.
by Todd Austin and Sasha Erickson
How to Create a Culture that Keeps Your Employees from Breaking Up with You
Healthcare employees admit that the 3 main factors contributing to the most stress at work are:
-
- Concerns about being trainied for the required workload
- Worries about job security
- Finding the time to balance work and personal life
As a result, almost 60% of those working in the healthcare space reported their self-assessed level of burnout to be between moderate and very high—which can be attributed to the high-level emotional investment required for the job.
While the long-term and post-acute care is one of the fastest growing industries in the nation, it also ranks in the top 5 workforces with the highest turnover.
Fortunately, the care employee burnout crisis is fixable.
The cure?
Treating our staff, and ourselves, with a little more conscious compassion.
The Long-Term Effects of Unappreciation
For most other industries, employee turnover peaks at one year.
But for the long-term and post-acute care industry, 40% of turnover occurs within an employee’s first 100 days.
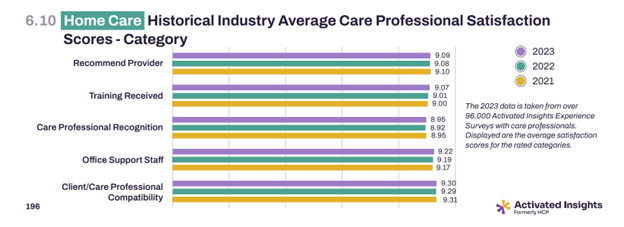
Which isn’t leaving much room for providers to retain their staff. According to the 2024 Activated Insights Benchmarking Report, annual care staff turnover increased by 14% within the last two years, averaging a total of 79.2%.
But there is hope in the data.
What if we told you that simply thanking your care staff more could get them to stay longer than 3 months?
According to the Benchmarking Report, recognition received the lowest satisfaction score from employees. Care staff are most dissatisfied with the appreciation they’re receiving after a job well done, followed by feeling inadequately prepared for the field.
Not only are feelings of unappreciation causing turnover rates to skyrocket, it’s also having a detrimental impact on the state of the industry.
As a result of not feeling appreciated or recognized for the work they do, your employees may be showing warning signs of impaired grief processing:
-
- Irritability or anger
- oddly negative behaviors or attitudes that are uncharacteristic for the employee
- Obsessive thoughts
- rumination over certain patients or issues that is constantly brought up and seems to never be resolves
- Hyper alertness or overreactive behaviors
- intense, erratic behaviors or excessive attention to work that is unwarranted or outside of the normal response
- Self-harming behaviors
- gravitation to overworked, exhaustive behaviors e.g. refusing to take breaks, taking on added tasks unnecessarily
- Apathy or numbness
- lack of reaction to items that would normally cause a response, decrease in emotions, or refusal to address difficult emotions
Contrary to popular opinion, an employee doesn’t leave their emotions at the door when they come into work. Especially if they work in a service-based industry like long-term and post-acute care.
The emotions an employee feels while caring on the job affects performance, customer and employee satisfaction, and care outcomes.
For example, if an employee is feeling stressed, frustrated, or disgruntled, they will either appear as they’re caring for their residents and patients or be forced to put up a positive front on the outside while bottling up negative emotions on the inside. Whether these types of negative emotions are revealed in the open or held within, either outcome leads to low satisfaction and high employee turnover.
Instead, be an advocate for your employees’ wellbeing and mental health. Provide resources for mental health support and regularly check-in with your staff at important milestones. Offering competitive benefits, flexible hours, and paid time off encourages employees to tend to their own needs as well as others.
As a highly accomplished executive, Todd Austin, COO & President of Activated Insights, is recognized as a leading voice in the rapidly-growing care industry. With over a decade of experience in executive leadership roles, Todd brings a wealth of knowledge and expertise to his current position as a key member of the Activated Insights team.
With a background in sales, marketing, management, operations, and finance, Todd is a true Renaissance executive with a rare combination of strategic and tactical skills. His expertise in developing and implementing growth strategies, optimizing operations, and driving profitability has made him a sought-after advisor to many organizations.
Sasha Erickson is the Director of Talent at Activated Insights, formerly HCP. With over 10 years of experience in human resources across a variety of industries, Sasha has worked with organizations ranging from small businesses to Fortune 500 companies. She graduated Summa Cum Laude from Utah State University with a degree in Business Administration and minors in Human Resource Management, Marketing, and Finance.
Sasha’s career history includes roles at Avant Guard Monitoring Centers, Goldman Sachs, Schreiber Foods, JBS and Pilgrim’s Pride Corporation, RR Donnelley, and Denver Public Schools. Her expertise spans talent acquisition, employee engagement, culture development, HCM software implementation, and strategic HR management.
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Rowan Report | Jul 12, 2024 | Partner News
by Bud Meadows, CEO, Activated Insight
I am thrilled to announce that we are now consolidating our growth under one unified name: Activated Insights. This new name clearly reflects our dedication to serving the long-term and post-acute care market, and it better represents our diverse range of unique capabilities.
As we transition to Activated Insights over the coming months, you’ll benefit from our integrated capabilities designed to empower employees to deliver the very best care, and make clients feel like they’re receiving just that. And we’re committed to doing our part by:
-
Providing you with the data to help recruit and retain employees.
-
Educating and supporting your clinical and care staff.
-
Enabling you to improve the experience of the people in your care through our unique analytics, workflow, and benchmarking.
-
Informing and enhancing internal processes so you can demonstrate your commitment to those you hire and serve.
Although we are adopting a new name, the heart and mission of who we are remains the same. We are dedicated to helping you make the most of every interaction for your employees, clients, and beyond.
Our goal is to keep you well-informed and ensure your experience with us remains seamless throughout this transition. You can expect to see updated branded materials in the coming months.
Bud Meadows
Chief Executive Officer, Activated Insights, Formerly HCP
by Elizabeth E. Hogue, Esq. | Apr 11, 2024 | Clinical, Regulatory
By Elizabeth E. Hogue, Esq.
A key purpose of the Health Insurance Portability and Accountability Act (HIPAA) is certainly to protect patient information. Another is to help ensure that patients have access to their health information. In fact, the Office of Civil Rights (OCR) of the U.S. Department of Health and Human Services, the primary enforcer of HIPAA, has focused on enforcement actions against providers that do not make information available to patients on a timely basis. OCR launched a right to access enforcement initiative in 2019 that is continuing.
Providers must give medical information to patients and their representatives within thirty days of requests. When they fail to do so, they may be subject to enforcement action by OCR. Following are two examples of recent enforcement actions.
OCR announced on April 1, 2024, that Essex Residential Care in New Jersey will pay a civil money penalty of $100,000 to resolve violation of HIPAA’s right of access standard. This is the 48th settlement reached under the right of access initiative. OCR received a complaint in May of 2020 from the personal representative of the estate of a patient who passed away. Following an investigation by OCR, the personal representative, who was the son of the patient, received the records in November of 2020. The provider did not contest the fine.
In another recent case, the daughter of a patient who passed away was appointed as the personal representative of her mother’s estate. She made multiple requests to Phoenix Healthcare for a copy of her mother’s medical records. She finally received the records one year after her initial request. Phoenix Healthcare initially received a civil money penalty of $250,000 for failure to provide timely access.
The provider appealed. An administrative law judge (ALJ) upheld the violation and ordered Phoenix to pay a civil money penalty of $75,000. The Departmental Appeals Board affirmed the ALJ’s decision. Then Phoenix agreed to settle for $35,000 and waived the right to further appeals. While it may seem in this case that the provider’s appeals significantly lowered its costs, it is important to note that the provider also undoubtedly expended significant resources on two appeals of OCR’s enforcement action.
Providers have placed a great deal of time and effort into the protection of healthcare information in compliance with HIPAA. Rightfully so, but providers seem to have lost sight of the fact that HIPAA is also about ensuring that patients and their representatives have timely access to their records. Now is the time for providers to conduct intensive education of staff members about HIPAA’s requirements regarding access in order to avoid enforcement actions like those described above.
©2024 Elizabeth E. Hogue, Esq. All rights reserved. No portion of this material may be reproduced in any form without the advance written permission of the author. For more information on how to get access to this or any other article, please contact The Rowan Report.
by Tim Rowan | Apr 11, 2024 | Clinical, Editorial, Telehealth
by Tim Rowan, Editor Emeritus
In 2020, doctors flooded telehealth companies with requests for help caring for patients reluctant to leave home to come to their appointments. Following suit, many Home Health agencies that had never considered investing in home telehealth before, opened up their wallets to acquire equipment, from simple wearables to high-end, HIPAA-compliant video systems.
In addition to the need to provide care at a safe distance, many HHA leaders knew the added service would attract the attention of hospitals desperate to discharge recovering Covid victims as well as non-Covid patients. Some HHAs established relationships with hospitals they had not had before, given the chance to demonstration Home Health’s unique advantages over extended hospital stays and discharges to institutions such as SNFs that had become virtual death sentences during the height of the pandemic.
All Things Must Pass
 With the introduction and widespread free availability of Covid mRNA vaccines, the death rate graph line began to tilt downward. Then came the discovery that the SARS-CoV-2 and its variants are transmitted through the air and not through unwashed surfaces. People stopped disinfecting their counter tops after unloading groceries. And they started in-person doctor visits again. Patients returned to allowing nurses into their homes.
With the introduction and widespread free availability of Covid mRNA vaccines, the death rate graph line began to tilt downward. Then came the discovery that the SARS-CoV-2 and its variants are transmitted through the air and not through unwashed surfaces. People stopped disinfecting their counter tops after unloading groceries. And they started in-person doctor visits again. Patients returned to allowing nurses into their homes.
In regions where vaccination and booster rates were high, hospitals found themselves with more and more empty beds. They took down tented treatment centers in their parking lots and sent refrigerated trailers back to trucking companies. Desperation referrals to Home Health tapered off, as did the need for virtual visits.
Isaac Newton said every action has an equal and opposite reaction. If that holds true in the healthcare business as it does in physics, the reaction to Covid easing is seen in Remote Patient Monitoring tech companies. According to Fierce Healthcare, the New York Stock Exchange told one RPM company, Amwell, formerly known as “American Well,” to raise its stock price or be delisted. Fierce added detail about the company’s woes:
“Despite decimating its workforce at the end of 2023 to cut expenses, the company still projects a 2024 loss between $160 million and $155 million amid incremental revenue growth. The company’s market cap was a stone’s throw from $6 billion at the height of its valuation, when shares were trading for more than $42 each. Amwell shares were trading at $0.72 as of market close on April 5, giving the company a current market cap of about $208.6 million.
Another market leader fared no better, Fierce Healthcare found. “Telehealth giant Teledoc, which has been in operation for 20 years, has struggled in the stock market and is facing headwinds as the virtual care market has become crowded with digital health players. Shares dropped 22 percent in February as the company missed fourth-quarter revenue estimates and offered a downbeat forecast for the rest of the year.”
Teledoc’s 15-year CEO, Jason Gorevic, resigned last week after the company reported a net loss of $220 million for 2023, following 2022’s historic loss of $13.7 billion, mostly from a write-off related to the plummeting value of its ill-advised Livongo acquisition. According to Fierce Healthcare, Teladoc shelled out $18.5 billion for the digital chronic condition management company, a record in digital health.
Gorevic’s rationale that the telehealth field has become too crowded may not be far off. Last July, Becker’s Hospital Review published an industry survey titled “280+ Telehealth Companies to Know.” The list included a half dozen names we recognized from past Home Health conferences, including Health Recovery Solutions, AMC, Vivify, and FoneMed.
Do Hospital Woes Translate Down to Home Health?
 Making comparisons between telemedicine companies that focus on hospitals and physicians and those who focus on post-acute providers is hampered by the fact that few in our sector are publicly traded and do not share their numbers. UnitedHealth, which acquired Vivify in 2019 and assigned it to its Optum division, does not separately report Vivify revenue.
Making comparisons between telemedicine companies that focus on hospitals and physicians and those who focus on post-acute providers is hampered by the fact that few in our sector are publicly traded and do not share their numbers. UnitedHealth, which acquired Vivify in 2019 and assigned it to its Optum division, does not separately report Vivify revenue.
Health Recovery Solutions, one of the best-known names in post-acute RPM, is privately held by its founding CEO and seven investors. Its most recent influx of $800,000 occurred in January, 2022, making it impossible to determine whether it was motivated by investor confidence or the need for cash as Covid began its decline.
Analysis
This publication has promoted the advantages of remote patient monitoring for its entire 25-year existence. We have covered startups and established tech companies offering every technology from PERS to Zo monitors to automated phone calls, in-home cameras and microphones. We have followed the evolution of two-way communications and vital sign detectors from tabletop devices to tablets and smartphones. We have even tested a few robots. We have seen HHAs experience great success, and we have seen devices collecting dust on shelves.
Throughout, we have maintained that, when selected, implemented, and deployed properly, monitoring patients 24/7 instead of once or twice a week can improve patient outcomes, boost agency reputation, and, more often than not, produce a healthy ROI. The end of the latest pandemic may mean the end of demand for Remote Patient Monitoring systems, but that would be unfortunate.
 Tim Rowan is a 30-year home care technology consultant who co-founded and served as Editor and principal writer of this publication for 25 years. He continues to occasionally contribute news and analysis articles under The Rowan Report’s new ownership. He also continues to work part-time as a Home Care recruiting and retention consultant. More information: RowanResources.com or Tim@RowanResources.com
Tim Rowan is a 30-year home care technology consultant who co-founded and served as Editor and principal writer of this publication for 25 years. He continues to occasionally contribute news and analysis articles under The Rowan Report’s new ownership. He also continues to work part-time as a Home Care recruiting and retention consultant. More information: RowanResources.com or Tim@RowanResources.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com













 With the introduction and widespread free availability of Covid mRNA vaccines, the death rate graph line began to tilt downward. Then came the discovery that the SARS-CoV-2 and its variants are transmitted through the air and not through unwashed surfaces. People stopped disinfecting their counter tops after unloading groceries. And they started in-person doctor visits again. Patients returned to allowing nurses into their homes.
With the introduction and widespread free availability of Covid mRNA vaccines, the death rate graph line began to tilt downward. Then came the discovery that the SARS-CoV-2 and its variants are transmitted through the air and not through unwashed surfaces. People stopped disinfecting their counter tops after unloading groceries. And they started in-person doctor visits again. Patients returned to allowing nurses into their homes. Making comparisons between telemedicine companies that focus on hospitals and physicians and those who focus on post-acute providers is hampered by the fact that few in our sector are publicly traded and do not share their numbers. UnitedHealth, which acquired Vivify in 2019 and assigned it to its Optum division, does not separately report Vivify revenue.
Making comparisons between telemedicine companies that focus on hospitals and physicians and those who focus on post-acute providers is hampered by the fact that few in our sector are publicly traded and do not share their numbers. UnitedHealth, which acquired Vivify in 2019 and assigned it to its Optum division, does not separately report Vivify revenue.


