What can Providers Give to Patients, Part 7
by Elizabeth E. Hogue, Esq.
What Providers can Give to Patients
Providers, including marketers, are tempted to give patients and potential patients free items and services. While providers usually have good intentions, they must comply with applicable requirements.
OIG Advisory Opinion
This article provides an example from OIG Advisory Opinion No. 09-11 that shows how the OIG applies exceptions described in this series of articles.
A Case Example
The request for this Advisory Opinion was submitted by a hospital that provides free blood pressure checks to anyone who requests the service during certain hours. The hospital said that it does not advertise free blood pressure checks, which are provided by a member of the nursing staff who follows specific guidelines and procedural checklists.
The hospital also said that free blood pressure checks are not conditioned on use of any other goods or services from the hospital or any other particular provider. No discounts are offered for follow-up services. Recipients of blood pressure checks are advised to see their own practitioners when results are abnormal. The hospital does not bill any payor, including the Medicare and Medicaid Programs, for this service.

OIG Analysis
In its analysis, the OIG first referenced the exception for preventive services described in Part 5 of this series.
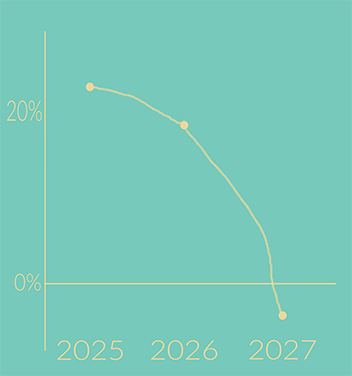
The OIG then pointed out that the fair market value of this service, especially if recipients use the service more than once, may exceed the limits of $15 per service or $75 per year described in Part 2 of this series. Therefore, said the OIG, the services may constitute a kickback.
According to the OIG, blood pressure checks are preventive services. The key question, however, is whether the free care promotes the provision of other, non-preventive care reimbursed by the Medicare and/or Medicaid Programs.
Is It Promotional?
In this case, the OIG said that it is unlikely that free blood pressure checks will result in the provision of other services. The factual basis for this conclusion in the Advisory Opinion was that the hospital did not:
- Make appointments with its practitioners for individuals with abnormal results
- Offer individuals discounts for additional covered services
- Otherwise promote its particular programs
Crafted with Care
“In sum,” said the OIG, “the Arrangement is appropriately crafted so as to avoid improper ties to the provision of other services…For these same reasons, we conclude that we would not impose administrative sanctions arising in connection with either the anti-kickback statute or the CMP on the Hospital in connection with the Arrangement.”
Final Thoughts
The 7 parts of this series describe and summarize the laws and exceptions to providing incentives, gifts, and help to patients in accordance with the Anti-Kickback Statute and the Civil Monetary Penalties Law. As long as you are following these regulations, providers should certainly use all of the exceptions available to them to provide better quality of care for patients.
# # #


Elizabeth Hogue is an attorney in private practice with extensive experience in health care. She represents clients across the U.S., including professional associations, managed care providers, hospitals, long-term care facilities, home health agencies, durable medical equipment companies, and hospices.
©2025 Elizabeth E. Hogue, Esq. All rights reserved.
No portion of this material may be reproduced in any form without the advance written permission of the author.
©2025 by The Rowan Report, Peoria, AZ. All rights reserved.