by Kristin Rowan | Nov 8, 2023 | CMS, Regulatory
By Kristin Rowan, Editor
On November 1, CMS issued its Home Health Final Rule for CY 2024. As expected, the final rule includes drastic pay cuts to Medicare home health services payments. The original proposed rule issued earlier this year included a 5.653% rate reduction, the remainder of the 7.85% reduction from 2020-2021 and an additional 1.636% for 2022, for a total rate reduction of 9.36% overall from the start of PDGM. In a surprising turn, CMS has not implemented the full 5.779% rate cut from the initial proposal, opting instead to introduce the rate cuts over two years. The 2024 rate cut will be 2.890%, half of the full adjustment CMS alleges is still needed. The CMS final rule does not attempt to collect any of the alleged overpayments from 2020-2022, totaling $3,439,284,729.00.
NAHC President Bill Dombi offered this response:
“We continue to strenuously disagree with CMS’s rate setting actions, including the budget neutrality methodology that CMS employed to arrive at the rate adjustments. We recognize that CMS has reduced the proposed 2024 rate cut. However, overall spending on Medicare home health is down, 500,000 fewer patients are receiving care annually since 2018, patient referrals are being rejected more than 50% of the time because providers cannot afford to provide the care needed within the payment rates, and providers have closed their doors or restricted service territory to reduce care costs. If the payment rate was truly excessive, we would not see these actions occurring. The fatally flawed payment methodology that CMS continues to insist on applying is having a direct and permanent effect on access to care. When you add in the impact of shortchanging home health agencies on an accurate cost inflation update of 5.2% over the last two years, the loss of care access is natural and foreseeable.
We now implore Congress to correct what CMS has done and prevent the impending harm to the millions of highly vulnerable home health patients that depend and will depend in the future on this essential Medicare benefit. Fortunately, longstanding advocates for home health care, Senator Debbie Stabenow (D-MI) and Senator Susan Collins (R-ME) have introduced S. 2137 to eliminate the rate cuts. We urge the Congress to support this legislation and enact it into law before the end of the year. The 2024 rate cuts must not take effect.”
The final rule includes the following:
- A net 3.0% inflation update
- A 2.890% Budget Neutrality permanent adjustment
- A $3,489,523,364 alleged overpayment in 2020-2022. CMS has not scheduled a collection of the alleged overpayment in 2024 or any other year yet.
- Recalibration of the 432 case mix weights with a separate budget neutrality adjustment in the payment rates of +1.0124%
- CMS estimates an increase in CY2024 Medicare spending of $140 million ($525 million inflation increase minus the $455 million rate adjustment plus a $70 million outlier FDL change)
HHAs that fail to provide required quality data will have these rates reduced by two percent.
Non-payment-related changes
In addition to the inflation increase and payment adjustments, the CMS Final Rule includes a number of other changes. These changes include amendments for the payment of Disposable Negative Pressure Wound Therapy, removing and replacing OASIS measures in HHVBP, new coverages and payments in IVIG services, the adoption of two new measures and the removal of one existing measure in HHQRP, coverage for lymphedema therapy items under a new Medicare Part B benefit, and revisions to Medicare provider enrollment requirements.
Hospice Provisions
Hospice Special Focus Program (SFP)
CMS is pushing forward with the Hospice SFP. Despite the commonsense suggested changes requested by NAHC and multiple others, CMS is using a flawed algorithm in the structure and implementation of SFP. This flawed algorithm will fail to identify hospices most appropriate for additional oversight and support. This creates the risk of reducing access to higher quality care and directing patients and families to hospices that perform most poorly relative to health and safety requirements. The official stance from NAHC is strong support of the SFPs goal to improve poor performing hospices, but are emphatically against the method in which SFP is being implemented and will continue to advocate for changes to the structure of the program.
Hospice Informal Dispute Resolution (IDR)
The IDR process for hospice is for condition-level survey findings which may trigger an enforcement action. The finalized IDR process allows hospice programs an opportunity to resolve disputes during recertification or reaccreditation for continued participation in Medicare. this allows for settlement agreement prior to a formal hearing, which will save time and money for the hospice agency. NAHC has additional recommendations for the Hospice IDR process that have not been implemented in the final rule.
Hospice 36-month rule
CMS is extending the “36-month” rule that currently applies to home health agencies and hospices, which is designed to prevent the flipping of Medicare certifications to non-vetted hospice owners. There are several exceptions to the rule for hospices. Even if a hospice undergoes a CIMO, a new owner must enroll as a new hospice and undergo a survey or accreditation unless:
- The hospice submitted 2 consecutive years of full cost reports since initial enrollment or the last CIMO, whichever is later.
- A hospice’s parent company is undergoing an internal corporate restructuring, such as a merger or consolidation.
- The owners of an existing HHA are changing the hospice’s existing business structure (for example, from a corporation to a partnership (general or limited)), and the owners remain the same.
- An individual owner of an hospice dies
New hospice owners will immediately be placed into the “high-risk” category for screening requirements and will have to submit fingerprints for a national background check from all owners with a 5% or greater direct or indirect ownership interest.
CMS Final Rule Synopsis and NAHC Response
We reached out to NAHC President Bill Dombi after the release of the Final Rule for CY2024. He provided us with a full breakdown of each provision in the final rule and the NAHC stance on each topic.
You can read all of these changes and how NAHC will continue to advocate for changes to the final rule here.
# # #
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently started writing for The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2023 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. homecaretechreport.com One copy may be printed for personal use: further reproduction by permission only.
editor@homecaretechreport.com
by Kristin Rowan | Oct 25, 2023 | Admin, Regulatory
by Kristin Rowan, Editor
Marking a significant victory for the HCAOA Connecticut Chapter and the home care industry, in the legislative session that ended last week, lawmakers unanimously passed a bill to reverse the policy guidance issued by the Department of Consumer Protection in January that banned use of the word “care” by home care agencies. In response to the guidance that directly harmed the industry, the Chapter and its members engaged in a strong lobbying effort to reverse it.
The guidance had caused significant concern and confusion for agencies, caregivers, consumers and lawmakers. Indeed, the Department had recently begun enforcing the ban against HCAs, requiring them to remove the word “care” from websites and other advertising.
On June 2, the state Senate gave final legislative approval to House Bill 5781, which allows HCAs to use the word “care” in their business names and advertising and advertise having employees trained to provide services to individuals experiencing memory difficulties as long as the agency prominently advertises that it solely provides nonmedical care, and doesn’t use any words, such as those related to medical or health care licensure or services, to describe services beyond the scope of those a HCA is authorized to provide. Also, HCAs must give consumers written notice that the agency provides nonmedical care and obtain the consumer’s signature on the notice before providing services. The Governor is expected to sign Public Act 23-48 shortly.
Chapter leaders and many members testified in support of the legislation, contacted the Governor and met with lawmakers and other officials, engaged in grass roots support, and advocated for the change. “It was a significant effort by the Chapter but our strategy and the work of members paid off,” said Marlene Chickerella, Chapter Chair and owner of B&M Homemaking Services in West Haven. “We are very grateful to lawmakers for changing the policy and appreciate all the support and assistance of our member-home care agency owners. They stepped up and clearly made a difference.”
Additionally, House Bill 5781, which originally arose out of the Homemaker-Companion Task Force recommendations:
• Requires the Office of Policy and Management to develop a plan and proposed timeline to transfer oversight of HCAs from Consumer Protection to the Department of Public Health; the plan will include recommendations on training standards and appropriate use of the term “care” to describe home care services.
• Adds failure to give a consumer written notice that the agency provides nonmedical care to a list of violations for which DCP may revoke, suspend, or refuse to issue or renew a HCA’s registration; requires DCP to revoke a HCA’s registration if the agency is found to have violated any revokable provisions three times in a calendar year.
• Requires HCAs to develop in consultation with the consumer a service plan or contract that includes (1) a person-centered plan of care, (2) anticipated oversight by the agency of the caregiver assigned to the consumer, and (3) how often the person who oversees the agency’s caregiver and consumer will meet.
• Requires DCP to post on its website a guide detailing the process for consumers to file complaints against a HCA; and requires agencies to give consumers a printed copy of this guide with their contract or service plan.
• Requires HCAs to create a brochure and maintain a website detailing the services it provides.
###
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly at kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
by Rowan Report | Oct 11, 2023 | CMS, Medicare Advantage, Regulatory
NOW AVAILABLE IN iQIES – Preview Reports and Star Rating Preview Reports for the January 2024 Refresh
CMS just published updated measure for Home Health Outcome Information Set (Oasis) and all HH QRP claims-based measures. These updated measures are no based on the standard number of quarter.
For additional information, please see the HH Quality Reporting Training webpage and the Home Health Data Submission Deadlines webpage.
©2023 by Rowan Consulting Associates, Inc., Colorado Springs, CO. This article originally appeared in Home Care Technology: The Rowan Report. Click here to subscribe. It may be freely reproduced provided this copyright statement remains intact. editor@homecaretechreport.com
by Tim Rowan | Oct 11, 2023 | Product Review
Home Health owners are used to walking tightropes. Indeed, there are many they are forced to walk every year, if not more often. One tightrope is a daily one. It delineates the fine line between regulatory compliance and risking being accused of non-compliance — and Home Health has a lot of regulations.
Owners, CEOs, CFOs, and boards struggle with a policy of spending money to ensure compliance with regulations or risking the expense of fines and payment denials for being found to be out of compliance.
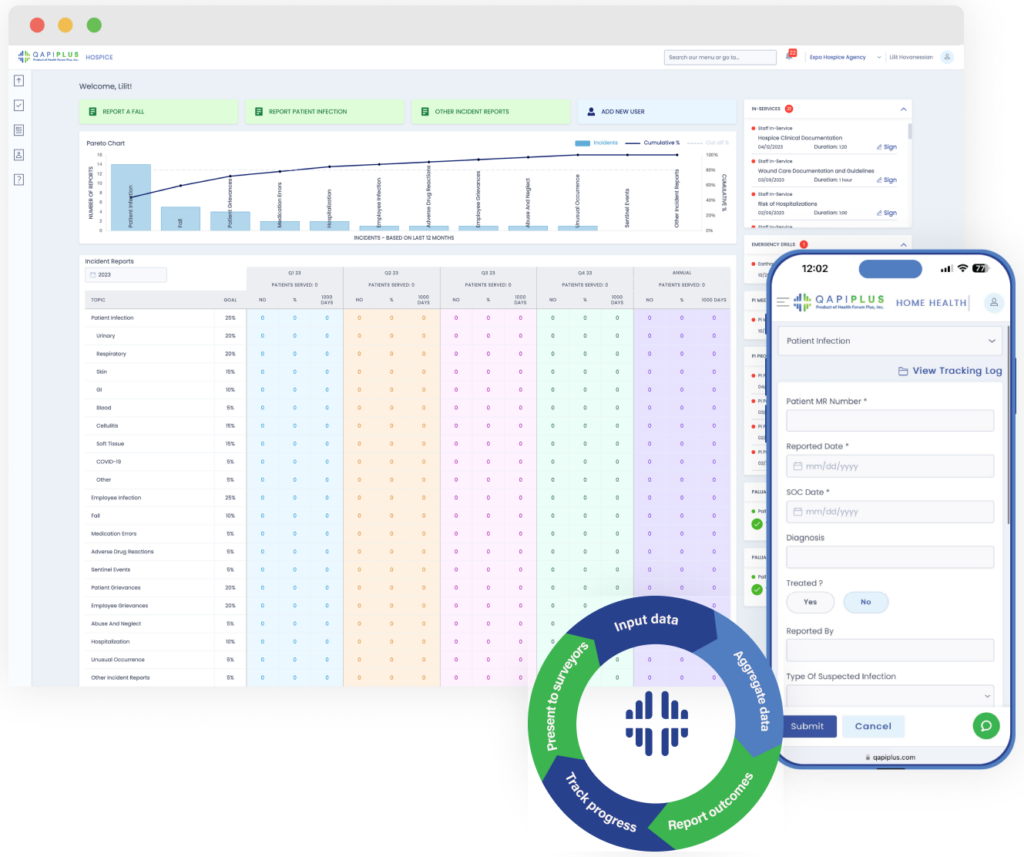
QAPIplus Automates Compliance
There may be a way to widen that tightrope to make it easier to walk. We participated in a product demonstration last week, courtesy of Armine Khudanyan, CEO/Founder, and Lara Koraian, Lead Software Developer, of QAPIPlus. In our view, automating the many processes involved in ensuring compliance should save many times the cost of a product such as this one. To date, however, we are not sure there is another product like this one.
Discussions of strategies to improve compliance occur during team and board meetings. Someone must know all the suspected deficiencies and assemble a meeting agenda. This is the first, and perhaps most important, piece that QAPIPlus automates. By drawing data from nearly every Electronic Medical Records product an HHA might be using, the tool identifies problem areas and creates a complete Quality Improvement meeting agenda, saving hours of work.
Management benefits from a clear, well-organized dashboard that can be customized to display the daily data each person in a position to monitor, flag, or improve compliance needs.
Items the software examines to alert staff about compliance problem areas include:
-
- Gaps in Emergency Management Planning
- Patient Infections
- Employee Infections
- Medication Errors
- Falls
- “Sentinel” events
- Patient Grievances
- Employee Grievances
- Abuse and Neglect
- Hospital Admissions
- Emergency Department Visits
- More
In addition to automating the assembly of meeting agenda items, QAPIPlus also builds in-service curricula. Recommendations for supplemental training can be used by the HHA or Hospice for individual or group training. The company, however, also offers online lessons, enough to cover most educational needs, from OASIS documentation to wound care.
Quick Clinician Training Modules
We were shown examples of 5-minute trainings — perhaps better described as reminders — that nurses like to use immediately before a visit. “For example,” CEO Armine Khudanyan offered, “a nurse knows a particular procedure will be required in the next patient home. He or she knows the procedure but has not done it in a long time. Our 5-minute “brush-up” can be viewed after parking in front of the patient’s home, and the nurse feels more confident going in.”
These lessons can also be given by Directors of Nursing or QA nurses to individuals who have an issue with some one regulation, perhaps a Condition of Participation about patient instructions, or about one OASIS item. Instead of dragging the entire clinical staff to one of those dreaded Saturday classes, the needed lesson is delivered to one person about one problem area.
QAPIPlus is the only quality management software solution to earn CHAP Verification and ACHC Certification for home health and hospice organizations. (The Joint Commission does not have a certification service.)
As is our custom, we rarely ask readers to take our word for it. The QAPIPlus leadership let us share a few quotes:
“I would like to thank you and the QAPIPlus platform for helping us achieve the GOLD seal of approval from The Joint Commission Triennial Survey. The surveyor was impressed with the program and the phone application. We were just cruising with the QAPI and in-service, the quickest and smoothest survey ever. Again, kudos to the team and developers. Such an amazing tool!”
Administrator, St. Agatha Home Health
“I have peace of mind that things are in order and that compliance is less of an issue to be concerned about.”
Director of Nursing, Home Health Agency
“The surveyor looked over the QAPIplus reports for about 15 minutes, and said ‘Okay, perfect. You guys have everything here,’ and that was that.”
Supervisor, Patient Care Services, Home Health Agency
This last comment brings up one final point that the QAPIPlus team said was important to make. “We have heard two types of comments from surveyors,” CEO Khudanyan added. “One is from surveyors who see the dashboard we customized just for them. They call it unique, easy to use, and comment on how much time it saves them to have everything in one place that they usually have to find by searching several applications on the screen and hundreds of papers in drawers. The second comment is from surveyors who walk into an HHA or Hospice after having used QAPIPlus at other agencies. They use words like ‘thank heavens’ when they see that this agency uses it too, knowing how easy their audit is going to be.” She added that it is hard to estimate the value of hosting a happy surveyor.
The Rowan Report rates QAPIPlus “worth serious consideration” for Home Health agencies and Hospices.
Tim Rowan is a 30-year home care technology consultant who co-founded and served as Editor and principal writer of this publication for 25 years. He continues to occasionally contribute news and analysis articles under The Rowan Report’s new ownership. He also continues to work part-time as a Home Care recruiting and retention consultant. More information: RowanResources.com
Tim@RowanResources.com
©2023 by Rowan Consulting Associates, Inc., Colorado Springs, CO. All rights reserved. This article originally appeared in Home Care Technology: The Rowan Report. homecaretechreport.com One copy may be printed for personal use; further reproduction by permission only. editor@homecaretechreport.com
by Rowan Report | Oct 4, 2023 | Admin, M&A
by Greg Schriber
In the dynamic landscapes of home health, home care, and hospice services, these industries are experiencing transformative trends, marked by evolving market changes and a surge in demand. Understanding these trends and strategically positioning one’s business for a lucrative sale is paramount. This article provides a detailed guide on understanding the current market landscape and optimizing business value for a successful sale.
Transformative Trends
The industry is witnessing a substantial increase in demand for home-based care services, primarily driven by an aging population and a growing preference for aging in place. This trend has been further propelled by the COVID-19 pandemic, as more families are opting for home care to mitigate the exposure risks associated with institutional settings. Additionally, the advent of technological advancements such as telehealth and health informatics is revolutionizing the way services are delivered, enhancing patient outcomes and operational efficiency. Embracing these innovative solutions is imperative to maintain competitiveness and address the changing needs of clients. The industry is also navigating through shifts in regulatory frameworks, emphasizing quality of care through value-based care models and patient satisfaction. Adherence to new regulations and standards is crucial to sustain the business and avoid penalties. Furthermore, the market is undergoing consolidation, with larger entities acquiring smaller providers to diversify their service offerings and extend their geographic reach. This trend poses both challenges and opportunities for business owners contemplating a sale.
Strategic Positioning for Sale
To position a business attractively for sale, optimizing operational efficiency is crucial. Streamlining operations and minimizing overhead costs not only enhance profitability but also make the business more appealing to potential buyers. Implementing industry best practices and leveraging technology can significantly elevate operational efficiency and service quality. Diversifying service offerings is another strategic move, as it can expand the customer base and open up new revenue streams. Providing a range of specialized and complementary services positions the business as a comprehensive solution, attracting acquirers. Building and maintaining a strong brand reputation through exemplary services, customer satisfaction, and community engagement is also vital. A reputable brand can draw in strategic buyers seeking market leadership. Investing in workforce development is equally important, as a skilled and stable workforce is a valuable asset that can influence business valuation positively. Maintaining financial health and accurate financial records is critical, as it demonstrates the business’s viability and can facilitate the due diligence process during the sale.
Managing the Sale Process
Seeking professional advice from industry experts, financial advisors, and legal counsel can offer invaluable insights and guidance throughout the sale process, aiding in accurate business valuation, negotiation of favorable terms, and navigation of legal intricacies. Negotiations require a strategic approach – understanding the buyer’s motivations, being transparent about expectations, and being willing to compromise can lead to a mutually beneficial agreement. Identifying a buyer whose vision aligns with that of the seller is essential to ensuring the continuity and growth of the business post-sale. Whether the buyer is a strategic entity looking to expand or a financial entity seeking investment opportunities, finding the right fit is crucial. Additionally, being well-prepared for the due diligence process can expedite the sale and reduce the risk of deal fallout. This includes organizing all necessary documents and addressing any potential issues beforehand. Developing a clear transition plan that involves open communication and support is essential to ensuring a successful handover and employee retention post-sale.
Positioning a healthcare business for sale is a multifaceted endeavor, involving operational optimization, brand enhancement, and meticulous strategic planning. By staying abreast of market trends, adopting best practices, and effectively navigating the sale process, business owners can maximize their business value and achieve a successful exit in this rapidly evolving industry. The journey extends beyond the sale; it’s about creating a legacy and ensuring the continued growth and service to the community under new ownership. By being proactive, strategic, and thoughtful, business owners can significantly impact the future of home-based care and improve countless lives.
Greg Schriber is the M&A Senior Advisor for American Healthcare Capital. To learn more about Transformative Trends, Greg can be reached at greg@ahcteam.com
©2023 by Rowan Consulting Associates, Inc., Colorado Springs, CO. All rights reserved. This article originally appeared in Home Care Technology: The Rowan Report. homecaretechreport.com One copy may be printed for personal use; further reproduction by permission only. editor@homecaretechreport.com
by Kristin Rowan | Sep 13, 2023 | Editorial, M&A, Regulatory
UnitedHealth Group Makes Bid to Buy Amedisys after Acquiring LHC Group
Amedisys is one of the leading providers of home health, hospice, and other healthcare at home services. It operates more than 500 locations in 37 states and the District of Columbia. After acquiring Contessa Health in 2021 for $250 million, Amedisys added hospital-at-home, SNF-at-home, and palliative care to its list of services.
Optum Outbids Option Care Health
In May of this year, Option Care Health and Amedisys issued joint statements announcing a merger of the two companies in an all stock-option bid. Option Care Health provides home and alternate site infusion services, while Amedisys provides home health, hospice, and high-acuity care. The merger was valued at $3.6 billion. It would have increased stockholder value, increased access to care across the United States, and created a network of more than 16,000 health care professionals, according to the joint statement.1
By June 26th, Option Care Health confirmed the termination of the merger and a $106 million termination payment from Amedisys, after Amedisys accepted an all-cash bid from UnitedHealth Group.2
UnitedHealth Expanding Service Options
UnitedHealth Group acquired LHC Group earlier this year for $5.4 billion.3 That acquisition folded LHC Group into UnitedHealth Group’s Optum. The acquisition came after increased demands for home care services. UnitedHealth Group considered this a move toward value-based care. The Federal Trade Commission stalled the merger with requests for additional details in mid-2022. Despite the FTC probe and a shareholder lawsuit, the deal was ultimately approved and the LHC Group delisted its stock on February 22.4
New Merger Faces Federal Scrutiny
Optum and Amedysis expected concerns over anti-trust issues surrounding the merger, according to a joint statement from the two groups. The Department of Justice recently asked for more information.5 The request will push back the timeline for the merger. Amedisys believes there is little geographic overlap between Amedisys and LHC Group and that the scrutiny is a result of other UnitedHealth Group acquisitions.
In a press release about the merger, Optum CEO Patrick Conway, M.D. said, “Amedisys’ commitment to quality and care innovation within the home, and the patient-first culture of its people, combined with Optum’s deep value-based care expertise can drive meaningful improvement in the health outcomes and experiences of more patients at lower costs, leading to continued growth.”6
Even with the recent acquisitions and mergers, if this deal with Amedisys proceeds, Optum will have only a 10% market share across the U.S. For this reason, as well as the demand for home care far exceeding the supply, Optum believes this merger will be approved.
Should a company that brokers health insurance also be allowed to be the provider of care? In this author’s experience, job-based healthcare insurance does not come with many options. There may be different levels of care to fit your budget, but the insurance company is already chosen by the employer. This means that employees and their families choose to have health insurance or not but cannot choose the insurance company.
Home Care, Hospice, Post-Acute Care, Palliative Care, and other in-home services are very personal. The company you choose and the care provider you get have to fit your needs and personality and there is a high level of trust needed to allow a stranger into your home when you are in a vulnerable state. If the insurance company is also providing the care, the option to find a care provider that suits the level of trust needed almost disappears.
In 2021, President Joe Biden signed an executive order for more vigorous oversight of the healthcare market. Mergers and acquisitions are being scrutinized more heavily to preclude monopolies of care. The FTC and DOJ, in response to this executive order, have proposed updates to antitrust guidelines that will make healthcare mergers and acquisitions more difficult.7
Medicare beneficiaries enrolled in Medicare Advantage has now reached 50%, making insurance companies more involved in senior care than ever before.8 Insurance companies only recently increased the percentage of revenue spent on patient care to 80%, up from as low as 50% before 2010.9 Given these facts, it may be worth questioning whether the insurance companies have too much control over care now, and if the acquisition of care providers by insurance providers should be eliminated completely to avoid a complete takeover of healthcare by insurance companies that already focus more on profit than people.
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Tim Rowan | Aug 23, 2023 | CMS, Regulatory
by Tim Rowan, Editor
Home Care Agency Removed Black and Hispanic Home Health Aides from Assignments to Accommodate Racial Preferences of Clients, Federal Agency Charges
There is a question that appears on social media chat pages with great regularity. What does a home care agency do when a client places it in a difficult legal position? The family of a Spanish-speaking grandmother asks for a Spanish-speaking caregiver. An elderly white gentleman insists on a white, English-speaking caregiver.
For agencies across the country, the only reasonable answer to this question is, “I don’t like my choices.” Those choices are to either offend, likely lose, a client, or risk violating Equal Employment Opportunity laws. It is common knowledge that home care clients have ample options should they become disillusioned with their current agency. In this situation, an agency has to choose between confronting a client’s racial bias and risk losing the client, or accommodating a client and losing a federal lawsuit. In other words, here we have the very definition of “no-win.”
With a recent action, the EEOC has put our entire industry on notice which option it expects. On July 31, the federal agency issued a public news release announcing it has filed a lawsuit against a New York agency. Four Seasons Home Care is a licensed personal care agency under a corporate umbrella with sister companies that offer Nursing and Rehabilitation, Certified Home Health, a Dialysis Center, Pharmacy, and an Adult Health Day Care Center. The company was faced with this common dilemma and made a choice of which the EEOC disapproved.
Reaction to the announcement, reprinted verbatim below, has already begun to appear on social media sites, including LinkedIn and home care groups on Facebook. One eloquent comment came from the CEO of an organization that serves an elderly client base made up of elderly people, mostly first-generation, who come from dozens of other countries and speak dozens of languages.
He pointed out that, in a diverse market like New York, it is common for patients and clients to express preference for an aide who can relate to their culture and speak their language. He even mentioned data that shows a connection between culture match and care effectiveness. The reason there has been a push to achieve diversity in the caregiving community expressly for the purpose of culture matching.
What stood out to this writer is that some of the language violates a journalistic rule, specifically the one against revealing the author’s bias within an otherwise facts-only story. In the second paragraph, the phrasing “including by removing Black and Hispanic” caregivers implies that the entire lawsuit is about disadvantaging these two groups. By looking beyond any implied meaning and parsing the language as written, one can see that removing these two specific ethnic groups is part of the accusation, but the writer offers no clue as to whether “part of” means 10 percent or 90 percent of the people discriminated against were Black and Hispanic.
Without this knowledge, one is led to assume that the entire accusation is that Four Seasons discriminated against Black and Hispanic caregivers. However, it is just as possible, based on the vague term “including,” that other ethnic groups were also victims of discrimination. It is just as possible that some Black and Hispanic caregivers were recipients of bonus work hours when assigned to clients who requested a caregiver with their cultural or language backgrounds. Sadly, the bottom line is that the language of the news release does not actually say what it appears to say. We will have to wait for the case to arrive in court to know what percentage of Four Seasons policy discriminated against minorities and what percentage help them.
Complete Announcement From EEOC
NEW YORK — ACARE HHC Inc., doing business as Four Seasons Licensed Home Health Care Agency, a Brooklyn-based company that provides its clients with home health aides, violated federal law by removing aides from their work assignments due to their race and national origin to accommodate client preferences, the U.S. Equal Employment Opportunity Commission (EEOC) charged in a lawsuit filed today.
According to the EEOC’s lawsuit, Four Seasons routinely would accede to racial preferences of patients in making home health aide assignments, including by removing Black and Hispanic home health aides based on clients’ race and national origin-based requests. Those aides would be transferred to a new assignment or, if no other assignment were available, lose their employment completely.
Such alleged conduct violates Title VII of the Civil Rights Act of 1964, which prohibits employers from discriminating against employees on the basis of race and national origin.
The EEOC filed suit, (EEOC v. ACARE HHC d/b/a Four Seasons Licensed Home Health Care, 23-cv-5760), in the U.S. District Court for Eastern District of New York, after first attempting to reach a pre-litigation settlement through the agency’s conciliation process. The EEOC seeks compensatory damages and punitive damages for the affected employees, and injunctive relief to remedy and prevent future discrimination based on employees’ race and national origin.
“Making work assignment decisions based on an employee’s race or national origin is against the law, including when these decisions are grounded in preferences of the employer’s clients,” said Jeffrey Burstein, regional attorney for the EEOC’s New York District Office.
“It is long past the day when employers comply with the discriminatory requests of its clients or customers, to the detriment of its Black and Hispanic workers,” said Timothy Riera, acting director of the New York District Office.
The EEOC’s New York District Office is responsible for processing discrimination charges, administrative enforcement, and the conduct of agency litigation in Connecticut, Maine, Massachusetts, New Hampshire, New York, northern New Jersey, Rhode Island, and Vermont.
More information about race discrimination can be found at eeoc.gov/racecolor-discrimination. More information about national origin discrimination can be found at eeoc.gov/national-origin-discrimination.
The EEOC advances opportunity in the workplace by enforcing federal laws prohibiting employment discrimination. More information is available at eeoc.gov. Stay connected with the latest EEOC news by subscribing to our email updates.
Tim Rowan is a 30-year home care technology consultant who co-founded and served as Editor and principal writer of this publication for 25 years. He continues to occasionally contribute news and analysis articles under The Rowan Report’s new ownership. He also continues to work part-time as a Home Care recruiting and retention consultant. More information: RowanResources.com
Tim@RowanResources.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report.homecaretechreport.com One copy may be printed for personal use: further reproduction by permission only. editor@homecaretechreport.com
by Tim Rowan | Aug 9, 2023 | Editorial
analysis by Tim Rowan, Editor
It is good to occasionally remind ourselves that 2023 is the year enrollment in Medicare Advantage reached a full half of Medicare beneficiaries. Originally conceived as a plan to control spending, MA does seem to be achieving that goal.
At what cost, however?
The Medicare trust fund pays insurance companies participating in the MA program a per-patient-per-month fee based on the company’s own declaration of each customer’s health and likely future needs. With those monthly payments, MA companies provide care as needed. Or at least they are supposed to.
Frequently, since the program began, whistleblowers have told the government that employees are rewarded for increasing a patient’s risk-adjustment, the clinical assessment that is supposed to be scored by a physician but is often instead scored through data mining. That practice involves employees searching through patient records, looking for signs of health conditions that would raise their assessment, and thus their value to the insurer. In other words, a class of crime that would earn an HHA a hefty fine if they did it with their OASIS assessments.
Evidence has been mounting lately that these insurance companies not only fudge the numbers to gather more than they should from Medicare, but they also provide as little care as they can get away with. Our industry is familiar with the penny-pinching MA companies practice when authorizing in-home care. The problem is larger than that.
String of Recent Accusations
- The HHS Office of Inspector General issued a report revealing how Elevance, the company formerly known as Anthem, made $5.5 billion in profits in the first six months of this year, a 14.4% jump from the $4.8 billion in profits it made during the same period of 2022. The profits, OIG said, came mostly from denying care to Medicaid beneficiaries, care that their physicians had recommended.
- The largest insurer, with 27 percent of the market, UnitedHealth’s investors were distraught in June when it appeared the company was spending too much on patient care. Their fears were calmed, however, when United reported revenue of $56.3 billion for 2Q 2023, compared to $45.1 billion in the same quarter of 2022.
- Cigna is the target of a class action suit in California, in which it is accused of using an algorithm to deny care, overriding and sometimes ignoring physician recommendations.1
Last October, the New York Times summarized the problem with a list of recent government findings and accusations:
“Kaiser Permanente called doctors in during lunch and after work and urged them to add additional illnesses to the medical records of patients they hadn’t seen in weeks. Doctors who found enough new diagnoses could earn bottles of champagne, or a bonus in their paycheck.
“Elevance Health paid more to doctors who said their patients were sicker. And executives at UnitedHealth Group, the country’s largest insurer, told their workers to mine old medical records for more illnesses — and when they couldn’t find enough, sent them back to try again.
“Each of the strategies — which were described by the Justice Department in lawsuits against the companies — led to diagnoses of serious diseases that might have never existed. But the diagnoses had a lucrative side effect: They let the insurers collect more money from the federal government’s Medicare Advantage program.”
Comparison to Home Health and Hospice
Naturally, these examples reach into the hundreds of billions because MA covers hospital and physician claims, but the comparison to our sector is nevertheless valid.
Since payments to HHAs were first attached to patient assessments a quarter century ago, clinicians have gotten better and better at the task. OASIS assessments are more accurate and thorough than they used to be. Professional coders are more adept at identifying and sequencing appropriate diagnosis codes. AI-assisted tools entering the fray promise an enhanced level of accuracy. (See our product review of the most promising of these tools.)
From the beginning, more accurate assessments have always meant a 10 to 15 percent increase in an agency’s episodic payment over less accurate OASIS scores. Wary of being accused of upcoding, nurses have always been unnecessarily cautious with their intake assessments.
Upcoding Accusations
CMS has always responded to increasing accuracy with accusations of upcoding, even though the Medicare trust fund more often benefits from the above described undercoding habit. Regulatory adaptations have enshrined the fear of upcoding into an assumption that it will happen, with payments slashed in advance just in case it does.
When errors in assessments and claims are discovered by CMS contractors through sampling, the overpayment amount found in the sample is extrapolated to an agency’s entire patient census. The result has at times crossed the line into seven figures, with a payback demand that occasionally cripples the HHA.
Compare this practice to the gift given to MA companies that we revealed in these pages last February: “Government Lets Health Plans That Ripped Off Medicare Keep the Money” In researching that story, we found that CMS typically postpones its duty to audit the risk adjustment figures that MA plans submit annually. After getting more than a decade behind, they decided to write off overpayments to MA plans prior to 2018 and start auditing from that year forward.
As an additional gift they said they would demand repayments only on the amounts turned up in their sample dataset, without extrapolating to each MA’s total patient population as they do with HHAs.
What can one conclude from this comparison? Possibly that CMS is very good at policing millions of dollars but gets overwhelmed and gives up with amounts in the billions.
 Tim Rowan is a 30-year home care technology consultant who co-founded and served as Editor and principal writer of this publication for 25 years. He continues to occasionally contribute news and analysis articles under The Rowan Report’s new ownership. He also continues to work part-time as a Home Care recruiting and retention consultant. More information: RowanResources.com
Tim Rowan is a 30-year home care technology consultant who co-founded and served as Editor and principal writer of this publication for 25 years. He continues to occasionally contribute news and analysis articles under The Rowan Report’s new ownership. He also continues to work part-time as a Home Care recruiting and retention consultant. More information: RowanResources.com
Tim@RowanResources.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report.homecaretechreport.com One copy may be printed for personal use: further reproduction by permission only. editor@homecaretechreport.com
1 https://sharylattkisson.com/2023/08/class-action-suit-filed-against-cigna-over-alleged-use-of-algorithm-to-review-reject-patient-claims/
by Elizabeth E. Hogue, Esq. | Jul 12, 2023 | CMS, Regulatory
by Elizabeth Hogue, Esq.
For providers to be liable under the federal False Claims Act, enforcers must prove that they knowingly submitted false claims. The U.S. Supreme Court recently issued an opinion in United States ex rel. Schutte v. SuperValu, Inc. [No. 21-1326 (U.S. June 1, 2023)], which defines what “knowingly” means. The Court decided that providers act knowingly depending on their “culpable state of mind” when they submitted alleged false claims; not what providers may have thought after submitting them. The requirement to prove knowledge, or “scienter,” said the Court, refers to providers’ knowledge and subjective beliefs; not to what objectively reasonable persons may have known or believed.
On June 30, 2023, the U.S. Supreme Court issued orders that revive two whistleblower lawsuits based on the opinion described above. Specifically citing the above decision, the Court granted whistleblower Troy Olbausen’s request to hear his case. The Court then vacated an Eleventh Circuit decision that dismissed Olhausen’s whistleblower lawsuit.
The Eleventh Circuit previously dismissed Olhausen’s suit against Arriva Medical because he could not prove that the defendants had knowledge of their submission of false claims in view of their objectively reasonable interpretation of the Medicare rules in question. The Supreme Court sent the case back to the Eleventh Circuit for further consideration based on its decision in Schuttte v. SuperValu, above [Olhausen v. Arriva Med., LLC, No. 22-374 (U.D. June 30, 2023)].
Likewise, on June 30, 2023, the Supreme Court sent a case back to the Fourth Circuit for further consideration in light of the Schutte case.
These actions make it clear that the new standard set by the Supreme Court in the Schutte case will make a difference in cases based on the federal False Claims Act. The Court said in the Schutte case:
“Both the text and the common law also point to what the defendant thought when submitting the false claim – not what the defendant may have thought after submitting it…As such, the focus is not, as respondents would have it, on post hoc interpretations that might have rendered their claims accurate. It is instead on what the defendant knew when presenting the claims…Culpability is generally measured against the knowledge of the actor at the time of the challenged conduct.”
The Court also said:
“Under the FCA, petitioners may establish scienter by showing that respondents:
- actually knew that their reported prices were not their ‘usual and customary’ prices when they reported those prices;
- were aware of a substantial risk that their higher, retail prices were not their ‘usual and customary’ prices and intentionally avoided learning whether their reports were accurate, or
- were aware of such a substantial and unjustifiable risk but submitted the claims anyway…
If petitioners can make that showing, then it does not matter whether some other, objectively reasonable interpretation of ‘usual and customary’ would point to respondents’ higher prices. For scienter, it is enough if respondents believed that their claims were not accurate.”
Proving that providers submitted false claims just got tougher for enforcers.
See Ms. Hogue’s earlier report on this SCOTUS case in our June 7 edition: homecaretechreport.com/article/3587
©2023 Elizabeth E. Hogue, Esq. All rights reserved. No portion of this material may be reproduced in any form without the advance written permission of the author.
©2023 by Rowan Consulting Associates, Inc., Colorado Springs, CO. All rights reserved. This article originally appeared in Home Care Technology: The Rowan Report. homecaretechreport.com One copy may be printed for personal use; further reproduction by permission only. editor@homecaretechreport.com
by Tim Rowan | May 17, 2023 | Admin, Regulatory
by Tim Rowan, Editor
T
he Department of Labor, Wage and Hour Division, has selected several southeastern states as targets for its investigation into a practice that appears to be quite common, underpaying in-home caregivers. It appears, based on early DoL reports, that some Home Care agency owners in Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina and Tennessee either do not understand the law, or simply try to get away with it.
According to a mid-February, 2023 report:
“From 2020 to 2022, Wage and Hour Division investigators identified violations in nearly 89 percent of more than 1,200 home care and nursing care investigations. These reviews led the agency to recover more than $16.2 million in back wages and liquidated damages for more than 13,000 workers.
The department produced an instructional webinar on federal wage and hour regulations for home care, residential care and nursing care industry employers, workers and other stakeholders in the Southeast. “Caring For Those Who Care: Fair Labor Standards Act Requirements in the Care Industry,” is part of the DoL’s ongoing education and enforcement initiative to improve compliance in those states.
On October 13, 2022, the DoL published a Notice of Proposed Rulemaking to revise the Department’s guidance on how to determine who is an employee or independent contractor under the Fair Labor Standards Act. The NPRM proposes to rescind the rule, Independent Contractor Status Under the Fair Labor Standards Act (2021 IC Rule), that was published in the closing days of the previous administration, January 7, 2021, and replace it with an analysis for determining employee or independent contractor status that is more consistent with the FLSA as interpreted by longstanding judicial precedent. The Department believes that its proposed rule would reduce the risk that employees are misclassified as independent contractors, while providing added certainty for businesses that engage (or wish to engage) with individuals who are in business for themselves.
A DoL publication explained this targeted effort aligns with the agency’s initiative to protect essential workers in the Southeast. See an April 28 update on progress of the proposed rule here.
Writing for a Polsinelli Law firm bulletin, home care attorney Angelo Spinola stated, along with the caveat that this is not to be construed as legal advice, “The DOL is not required to give employers prior notice of an audit. In fact, WHD investigators often initiate unannounced investigations to observe normal business operations. As such, the best way to prepare for a DOL audit is to conduct regular and periodic internal audits of employment records and policies to ensure compliance with the FLSA. Internal audits typically include a review of exempt employee classifications, independent contractor classifications, payroll and time records, and FMLA and other leave law compliance. It is advisable to work with knowledgeable employment attorneys who can counsel employers on current wage and hour laws and best practices.”
Abuse Found to be Widespread
From 2020 to 2022, Wage and Hour Division investigators identified violations in nearly 89 percent of more than 1,200 home care and nursing care investigations. These reviews led the agency to recover more than $16.2 million in back wages and liquidated damages for more than 13,000 workers. In addition, the division assessed employers a total of $156,404 in civil money penalties. The February DoL report cited two recent North Carolina cases as examples of the practices it uncovered throughout the South:
Gentle Shepherd Care – which provides home healthcare services in the Charlotte area – failed to combine hours when employees worked at more than one of its locations during the same workweek. By doing so, the employer did not pay the affected workers their additional half-time premium rate for overtime for hours over 40 in a workweek. The Fair Labor Standards Act requires all hours worked in a workweek be combined when calculating wages, regardless of where employees performed the work. Back wages and liquidated damages recovered: $193,768 for 98 workers.
A separate investigation found Greenville”s At Home Personal Care paid employees straight-time rates for all hours worked, including hours over 40 in a workweek. By doing so, the employer did not pay the additional half-time premium rate for overtime as the FLSA requires. In addition, the employer failed to pay for travel time between the clients’ homes when the employees visited multiple clients during the same day. The agency also did not keep accurate records as required. Back wages and liquidated damages recovered: $187,148 for 28 workers.
North Carolina Wage and Hour Division District Director Richard Blaylock stated, “Workers who provide home healthcare services deserve to be paid every penny of their hard-earned wages as they care for our loved ones. When employers choose to ignore the law, they deny workers the wages they earned and need to support their families. Employers must use this investigation’s outcome as a reminder to review their pay practices to ensure they comply with the law.”
Employers can contact the Wage and Hour Division at its toll-free number, 1-866-4-US-WAGE. The division also offers online resources for employers, such as a fact sheet on Fair Labor Standards Act wage laws overtime requirements. Workers who feel they may not be getting the wages they earned may contact a Wage and Hour Division representative in their state through a list and interactive online map on the agency’s website. Workers and employers alike can help ensure hours worked and pay are accurate by downloading the department’s Android Timesheet App for free. Learn more about Wage and Hour Division.