Paul Joiner: On the Record
Adminby Kristin Rowan, Editor
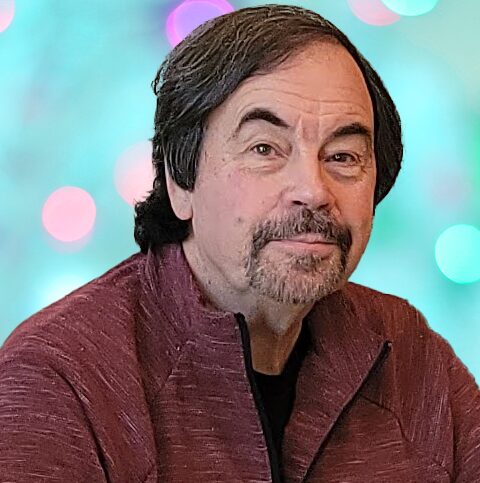
Paul Joiner
On the Record
Paul Joiner, CEO of HHAeXchange, sat down with The Rowan Report Editor Kristin Rowan to discuss the company’s new headquarters in Manhattan, the company culture he’s creating, his dedication to support those helping our most vulnerable populations.
In His Own Words
The Rowan Report: Paul, thank you for taking the time to talk to us. HHAeXchange is going through some significant growth recently. And now you’ve moved your headquarters from Long Island to Manhattan, correct? How did that decision come about?
Paul Joiner: HHAeXchange has been in Manhattan for a long time. Sandata, who we acquired earlier this year, was in Long Island. But, the move was planned with or without Sandata. We needed a nice sized space to convene people. We valued a large, multi-purpose meeting space over individual office space. It’s a space where the teams can meet when they come to town, where we can host clients, and larger company meetings.
RR: How does the new space support your team?
Paul: The majority of our team is remote. I don’t think remote work is healthy for everyone. It varies from person to person. It’s not a long-term healthy option. Returning back to the office 9-5 five days a week isn’t practical and not all that healthy either. We have created policies, a workspace, and a culture where people are invited to visit. Some come 2-3 days per week. Some only once a month. We maintain flexibility for our teams to work when and where they need to work. Being a single parent, for example, is really hard, so we stay flexible to support single parents to be where they need to be.
At the same time, we’ve seen the benefit of the connection and how much more healthy it is by physically coming together. For the younger workforce, they are enjoying getting together and coming into the office. We have to support our younger employees and their professional development. How do you professionally develop via Zoom or Teams? Physically coworking and promoting good and active environments compel people to come into the office. To build connections, you have to be together, not just on video.
RR: You have workers across the country, though. How does that work?
Paul: We have the main office here in Manhattan, a large and growing office in Minneapolis, and a smaller office in Miami. We try to keep people in areas that make it easy to meet. However, we do have some roles with certain criteria that allows for mostly remote work. Those teams come to one of the offices to meet when they can. We’ve hosted team meetings here and in Minneapolis recently.
RR: Has this new meeting space had an impact on the company culture?
Paul: Yeah, it has improved. We are having real, honest conversations about what needs to be improved. The team effort is the way we win and our teams understand that. We also understand that working hard doesn’t mean foregoing your life and the ability to recharge.
Work hard, be passionate, and motivate people with your mission and vision. The people we serve don’t have it easy, they are supporting the most vulnerable people.
RR: In a recent statement, you said that the new location will support collaboration and innovation. Do you have new features on the horizon? Are you investing in AI capabilities?
Paul: We have a lot in the works. We have a new mobile app in the beta phase that we’ll be rolling out that I’m really excited about. It’s actually an update, but it’s so massive that it’s basically new. We’re working on data analytics and data tracking for some of our largest clients. We’ve consolidated some screens into one spot to streamline and make the user more efficient. A lot of what we’re working on is foundational. We’re focusing on supporting companies as they scale.
RR: Are you looking into AI, either within the HHAeXchange platform, or in a partner?
Paul: Yeah, of course. AI is the future and it’s everywhere. We are looking at ways to return time to users, make it easier to train users, and make things easier on caregivers. We will try to generate more buzz around AI, but not until there’s real, tangible value. AI definitely needs to be part of our strategy, but being smart where we apply it to truly get the value-add for our clients. It has to improve the quality of life for the user. Does it improve the ability of caregivers to care for people?

RR: Do you have any additional acquisition or growth plans for the second half of 2025?
Paul: There’s a lot going on in the marketplace right now. A lot of our clients are growing really well also. So, we’re sort of in a heads-down mode. There’s a handful of things we’re looking at. Right now, I’m really excited about being a bigger participant across the full continuum of care for our populations. There are some opportunities to innovate and evolve to support integrated care over the next few years. I’ll just leave it at that…for now.
RR: Paul, thank you for joining me today. It’s always a pleasure.
# # #
About HHAeXchange
Founded in 2008, HHAeXchange is the leading technology platform for homecare and self-direction program management. Developed specifically for Medicaid home and community-based services (HCBS), HHAeXchange connects state agencies, managed care organizations, providers, and caregivers through its intuitive web-based platform, enabling unparalleled communication, transparency, efficiency, and compliance. In 2024, HHAeXchange expanded through the strategic acquisitions of Sandata, Cashé Software, and Generations Homecare System, strengthening its commitment to advancing the industry.
About Paul Joiner
Paul Joiner is an accomplished executive with extensive leadership experience in the healthcare sector. Currently serving as a Board Member at AssistRx, Joiner has held prominent positions, including Chief Executive Officer at both HHAeXchange and Kipu Health. Previous roles include Chief Operating Officer as well as Executive Vice President and General Manager at Availity, and Senior Vice President and General Manager of Health Plan. Joiner also served as Vice President of Client Engagement and Business Development at Midas+ Solutions, Xerox Healthcare Provider Solutions. Educational qualifications include a Master of Accountancy from Belmont University and a Bachelor of Accountancy from the University of Mississippi.


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com




 Earl L. “Buddy” Carter is an experienced businessman, health care professional and faithful public servant. For over 32 years Buddy owned Carter’s Pharmacy, Inc. where South Georgians trusted him with their most valuable assets: their health, lives and families. While running his business, he learned how to balance a budget and create jobs. He also saw firsthand the devastating impacts of government overregulation which drives his commitment to ensuring that the federal government creates policies to empower business instead of increasing burdens on America’s job creators.
Earl L. “Buddy” Carter is an experienced businessman, health care professional and faithful public servant. For over 32 years Buddy owned Carter’s Pharmacy, Inc. where South Georgians trusted him with their most valuable assets: their health, lives and families. While running his business, he learned how to balance a budget and create jobs. He also saw firsthand the devastating impacts of government overregulation which drives his commitment to ensuring that the federal government creates policies to empower business instead of increasing burdens on America’s job creators. Congressman Ami Bera, M.D. has represented Sacramento County in the U.S. House of Representatives since 2013. The 6th Congressional District is located just east and north of California’s capitol city, Sacramento, and lies entirely within
Congressman Ami Bera, M.D. has represented Sacramento County in the U.S. House of Representatives since 2013. The 6th Congressional District is located just east and north of California’s capitol city, Sacramento, and lies entirely within