Are Nurses Independent Contractors?
Adminby Kristin Rowan, Editor
Are Nurses Independent Contractors?
Jury will decide intent
After investigation, the U.S. Department of Labor (DOL) sued Amazing Care Home Healthcare Services over misclassification of workers, recordkeeping violations, damages, and unpaid overtime. The court decided the workers were misclassified.
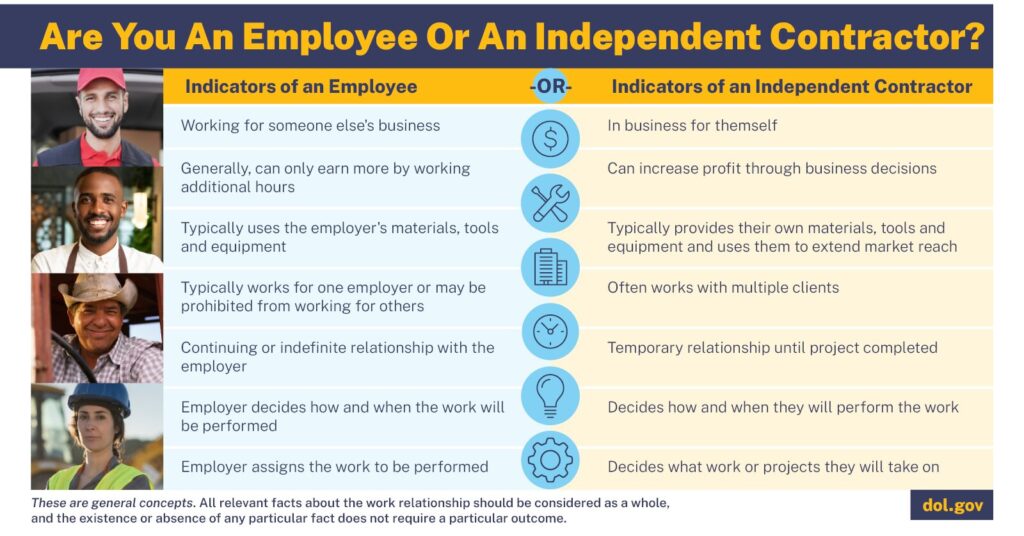
Classification as Employee
According to the decision, the workers were employees because the company had control over the work, set wages, required workers to report absences, and evaluated their performance. The DOL provides guidance on what constitutes an employee. Prior regulations use a “totality-of-the-circumstances” approach to classification, looking at the whole picture rather than a single determining factor. Other documents rely on an “economic reality” test that examines two core factors: the nature and degree of control a worker has over the work and the worker’s opportunity for profit or loss.
Summary Judgment
The DOL called for summary judgement, in which the judge would decide the case without a trial or jury due to “overwhelming” evidence. The judge partially agreed and granted summary judgement in favor of the DOL on worker classification, recordkeeping, and damages. The court declined summary judgement on the issue of overtime and intent. There is some question as to whether the workers were paid some overtime wages during the period in question and whether the misclassification was willful. These questions will be decided by a jury at trial.
Economic Reality
The totality framework to determine worker classification came into use during the Biden administration. The DOL has recently proposed a return to the economic reality framework from 2020. Two core and three additional factors comprise the economic reality test. These two core factors are the primary determinants:
- The nature of and degree of a worker’s control over their work
- does the employer control scheduling, pay rates, and prices;
- does the employer supervise performance and discipline workers
- Opportunity for profit or loss
- does the worker advertise services independently, negotiate contracts, decide when and where to work, have the ability to hire helpers to perform the work
These three additional factors are considered in classification analysis, but carry less weight than the two primary considerations:
- The amount of skill required for the work
- does the worker use their own specialized skills rather than relying on the company for training
-
- does the worker use that skill to grow the business
–and–
- The degree of permanence of the working relationship between company and worker
- is the work sporadic, as needed, or project-based
-
- is the company engaging in seasonal or temporary work or industry
–and–
- Whether the work is part of an integrated unit of production
- can the business operate without the work performed
Clear Answer
Using the economic reality test, can we classify home health nurses as independent contractors or employees without question?
Employee
Agency sets pay rate for the nurse
Supervised performance
Clients belong to the agency
Nurses do not hire and pay helpers
Nurses do not automatically make more when the agency grows
The business cannot operate without nurses
Independent Contractor
An agency could allow the worker to set their own schedule
Nurses use their own skills, degrees, and certifications
Work could be created as project-based where 1 client=1 project for 30 days
Final Thoughts
Without very careful planning and disruption of practice, it is pretty clear that home health workers are not independent contractors, but are employees. There may be significant differences in the operation of non-medical supportive care at home, but pay rates are still determined by the agency, performance is supervised, clients belong to the agency, and the business cannot operate without healthcare workers. The DOL sued for unpaid overtime amounting to $5.9 million on behalf of both LPNs and Home Health Aides.

If you do now or plan to in the future engage any worker as an independent contractor, review all current FLSA and DOL requirements to ensure you are not misclassifying your workers.
# # #


Kristin Rowan is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news. She is also a sought-after speaker on Artificial Intelligence, Technology Adoption and Lone Worker Safety. She is available to speak at state and national conferences as well as software user-group meetings.
Kristin also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. She works with care at home software providers to create dynamic content that increases conversions for direct e-mail, social media, and websites. Connect with Kristin directly at kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2026 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com