Advocacy Week
AdvocacyAdvocacy Week
FOR IMMEDIATE RELEASE
Contact: Elyssa Katz
communications@allianceforcareathome.org
571-281-0220
Over 240 Advocates Rally in DC for the Future of Care at Home
National Alliance for Care at Home Hosts Inaugural Advocacy Week on Capitol Hill
Alexandria, VA and Washington, D.C., September 12, 2025.
More than 240 care at home care advocates from across the country met with over 275 congressional offices this week to discuss key legislative and regulatory priorities for expanding access to home-based care services. The meetings were part of the 2025 National Alliance for Care at Home’s inaugural Advocacy Week.
Alliance Advocacy Week brings together leaders, advocates, and supporters to unite as one voice for care at home, driving positive legislative change and shaping the future of care to ensure broader access to the life-changing home care services for all Americans.
- Protecting home health care by preventing dangerous payment cuts
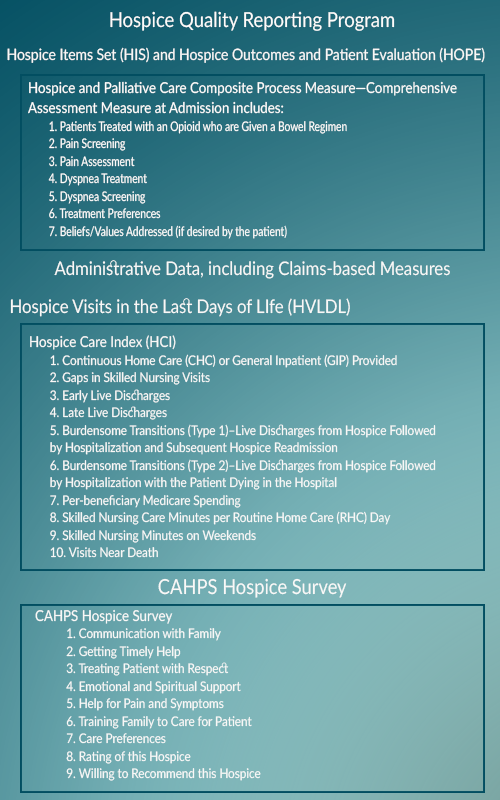
- Safeguarding the Medicare Hospice Benefit by ensuring hospice remains a separate holistic managed care model outside of Medicare Advantage
- Expanding telehealth access across many care at home services
- Supporting robust Medicaid HCBS funding to strengthen community-based care



In addition to Wednesday’s congressional meetings, Alliance Advocacy Week featured strategy sessions, beginner advocate training featuring a panel discussion with Congressional staffers, and in-depth policy briefings. On Thursday, the Alliance’s Assembly of State Associations – a network of leaders of state home care and hospice organizations – came together for a robust conversation.
The Alliance celebrates the achievements of this inaugural Advocacy Week on behalf of home-based care providers nationwide and will continue engaging in critical policy dialogue to support and expand access to essential care at home services.
# # #
About the National Alliance for Care at Home
The National Alliance for Care at Home (the Alliance) is the leading authority in transforming care in the home. As an inclusive thought leader, advocate, educator, and convener, we serve as the unifying voice for providers and recipients of home care, home health, hospice, palliative care, and Medicaid home and community-based services throughout all stages of life. Learn more at www.AllianceForCareAtHome.org.
©2025. This press release originally appeared on the National Alliance for Care at Home website and is reprinted here with permission. For questions or to request permission to use, please see press contact information above.