Alliance to Congress: STOP CUTS
Advocacy9% Cut Proposed
CMS proposed home health rule for 2026 includes disastrous cuts. A 3.2% market basket increase, a 0.8% productivity cut, a 5% reduction to recoup prior overpayments, and a 4.1% permanent reduction to prevent further overpayments. CMS proposed an additional 0.5% cut to account for high-risk outliers. In other words, CMS wants to pay less for all patients to make up for the small percentage of patients who need more care.
Deadline Looming
The mandatory comment period ended on August 29. Next, CMS reviews the submitted comments, responds to those comments (generally explaining why they are not going to listen), and then finalizes the 2026 rule. The final rule is due November 1, 2025. Although, that falls on a Saturday, so the deadline may extend to Monday. A good many of us will be in New Orleans for the Alliance annual conference and expo by then.
Group Effort
The National Alliance for Care at Home (Alliance) joined 150+ provider, patient, community, and advocacy groups to write a letter to Congress urging them to prevent the CMS proposed cut.
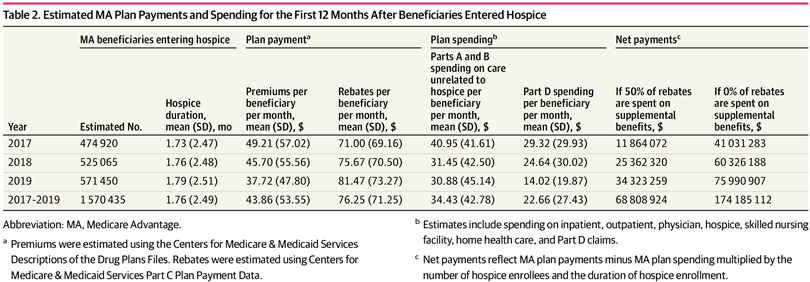
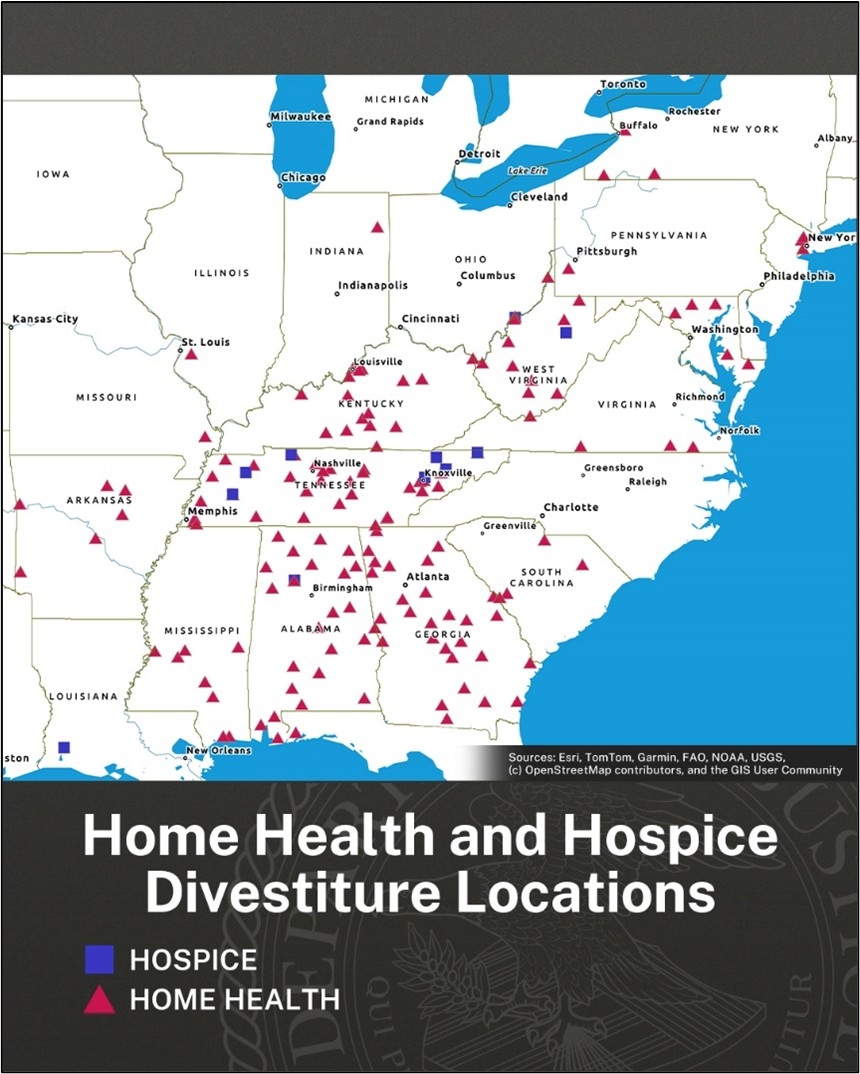
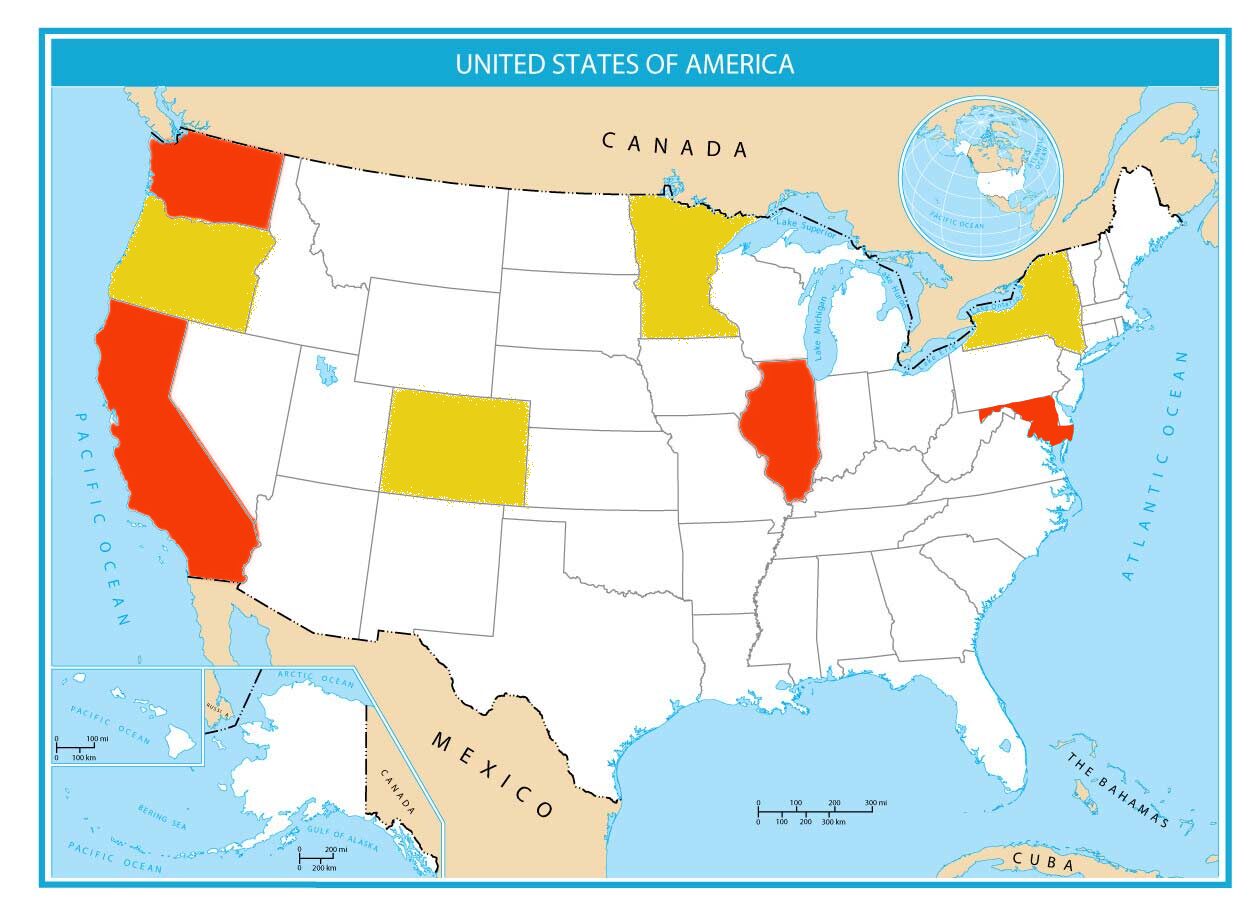
Pattern of Payment Reduction
The letter, addressed to Senate Majority Leader John Thune, Senate Minority Leader Chuck Schumer, Speaker Mike Johnson, and House Minority Leader Hakeem Jeffries, asks Congress to look at the consecutive years of pay reductions and how they have impacted home health. Because of the cuts, agencies have gone out of business or downsized, leaving rural areas without care.
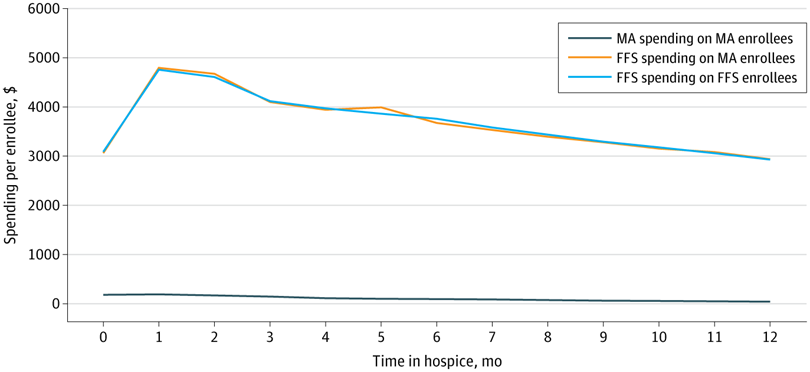
Home Health Costs Less
The letter also explains that cutting medicare payments actually costs more. When more patients have access to home health, CMS spends less on unplanned hospital visits and ER trips. Patients have fewer falls and accidents. Risk factors are identified earlier and preventative treatments are used before a patient’s condition requires hospitalization. Home health patients stay home years longer than those not receiving home health before entering a skilled nursing or assisted living facility.
What's at Risk
The Medicare Trust Fund, funded partially by payroll taxes, includes hospital insurance that pays for hospital (Medicare Part A) services. When these costs increase, the trust fund is at risk being insolvent and taxes are increased to put money back into the fund. Lowering home health payment rates and cutting off millions of people who depend on home health will impact tax payers as well.

# # #


She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com