UnitedHealth Group Acquisition of Amedisys Under Fire by DOJ
by Kristin Rowan, Editor
Justice Department Sues
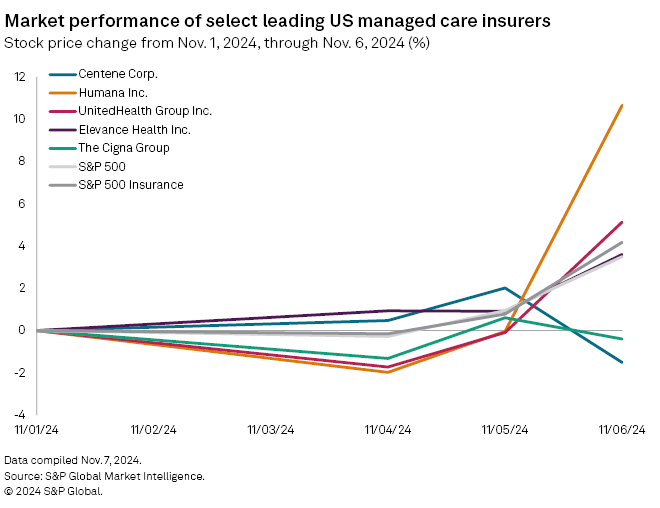
In September of 2023, UnitedHealth Group made a bid to purchase Amedysis. That acquisition has been under scrutiny since last year. When the bid was announced, the Department of Justice began an inquiry, asking for additional information. At the time, Amedysis indicated that they anticipated the inquiry.
Now, more than a year later, the Department of Justice, along with the Attorneys General of Maryland, New York, New Jersey, and Illinois, have filed an antitrust lawsuit to block the acquisition. The proposed $3.3 billion acquisition would eliminate competition between the two companies. It would also give too much control to UnitedHealth Group, according to the suit.
Statement from the Department of Justice
The DOJ and the Attorneys General stated that the merger is illegal. The two companies own so much of the market share in the space already that combining the two would mean less choice for patients and fewer employment options for nurses seeking competitive pay and benefits.
UnitedHealth Group already acquired Amedisys’s biggest home health and hospice rival, LHC Group. Since that acquisition, UnitedHealth Group and Amedisys have been two of the largest providers of home health and hospice care in the United States.

American healthcare is unwell. Unless this $3.3 billion transaction is stopped, UnitedHealth Group will further extend its grip to home health and hospice care, threatening seniors, their families and nurses.
Surprisingly, the former CEO and current board chairman of Amedisys acknowledged the problems. He said that the competition between the two companies has helped keep them honest. He also said it has driven better quality to the benefit of their respective patients. The former CEO went on to say that the companies also compete for nurses and the merger may threaten the benefits nurses receive. It seems even the heads of the companies involved know this is a bad idea.
UnitedHealth Group's Proposed Solution
In response to the concerns voiced by the DOJ, UnitedHealth proposed to divest some of its facilities to VitalCaring Group. UnitedHealth said this would prevent the monopoly the merger creates. The DOJ responded to that proposal somewhat harshly.
The complaint alleges that the UnitedHealth Group’s market share would be illegal in home health markets in 23 states and the District of Columbia. It would also be illegal in hospice markets in 8 states, and in the nurse labor market in 24 states.
UnitedHealth’s proposed divestiture would only alleviate the monopoly in a few areas. This leaves hundreds of markets across the U.S. in jeopardy. Further, VitalCaring Group has poor quality scores and is facing its own legal judgement of close to half a billion dollars. Allegedly, the current CEO of VitalCaring Group was the CEO of a competitor while running VitalCaring behind the scenes.
Good News for Home Health and Hospice
The complaint describes home health and hospice services as “critically important parts of the American healthcare system….Patients rely on the skill and expertise of home health and hospice nurses, who must effectively treat patients at home.
Millions of patients depend on United and Amedisys to receive home health and hospice care in the comfort of their homes. The Department’s lawsuit demonstrates our commitment to ensuring that consolidation does not threaten quality, affordability, or wages in these vital healthcare markets.
Attorney General Merrick B. Garland said, “We are challenging this merger because home health and hospice patients and their families experiencing some of the most difficult moments of their lives deserve affordable, high quality care options. The Justice Department will not hesitate to check unlawful consolidation and monopolization in the healthcare market that threatens to harm vulnerable patients, their families, and health care workers.”
Final Thoughts
Mister Attorney General, please turn your attention to CMS and Medicare Advantage, as they continue to threaten the safety and well-being of patients, families, and caregivers with increasingly low reimbursement rates and denials of coverage.
# # #


Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com