Medicare Home Health Cuts: Survey Says
FOR IMMEDIATE RELEASE
Contact: Elyssa Katz
571-281-0220
communications@
70% of Americans Oppose Medicare Home Health Cuts, National Poll Finds
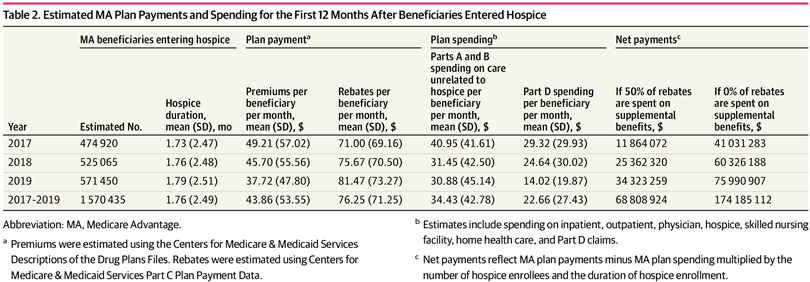
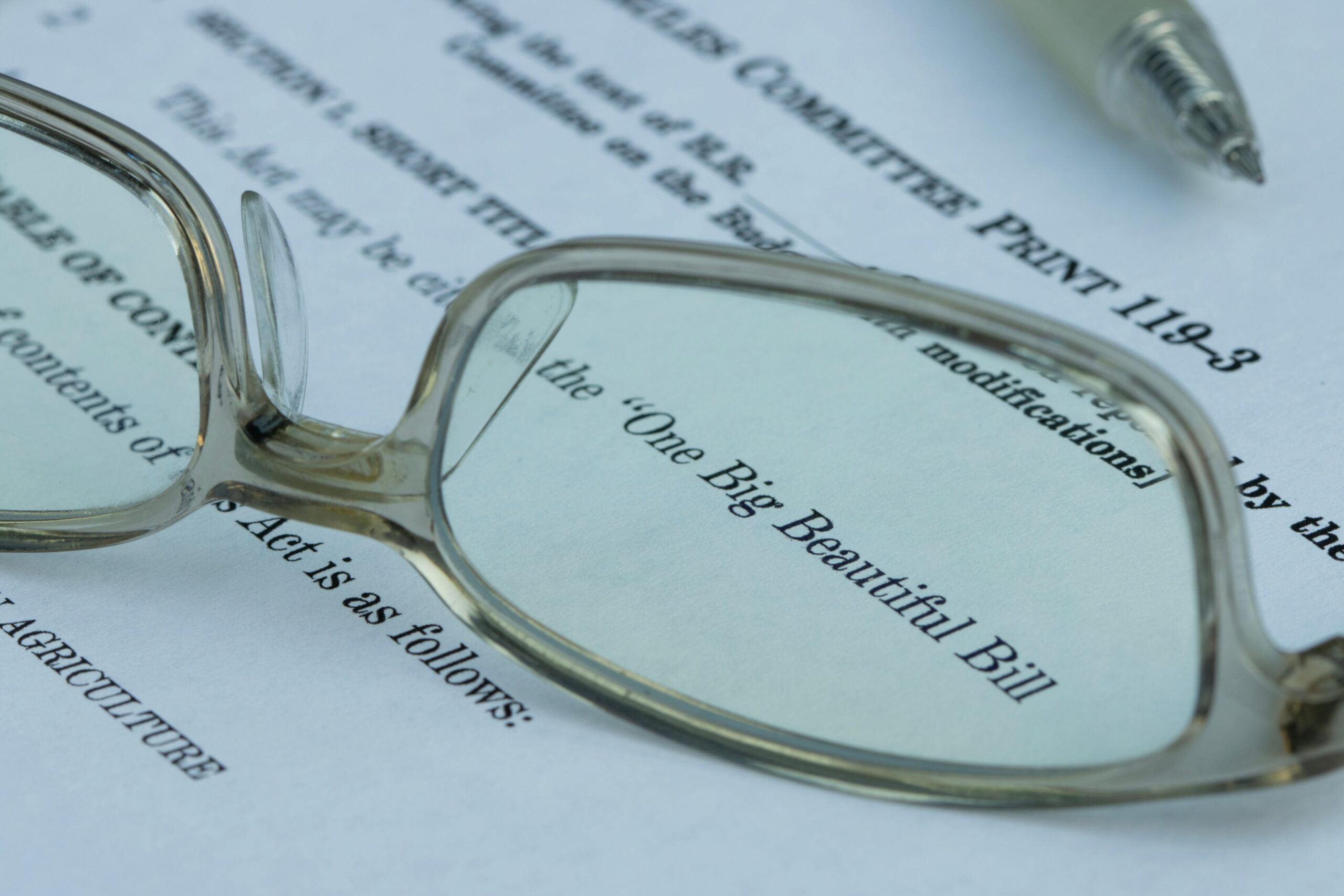
Alexandria VA, and Washington, DC, September 4, 2025– A new national poll by Fabrizio Ward, commissioned by the National Alliance for Care at Home (the Alliance), finds that seven in ten Americans oppose the Centers for Medicare & Medicaid Services’ (CMS) 2026 Medicare home health proposed rule, which would slash Medicare home health funding by an additional 9%, or $1.1 billion, next year. These cuts would put lifesaving home health care for millions of Americans at risk, particularly seniors and those with disabilities, while doing nothing to address fraud, waste, and abuse occurring in the home health payment system.
In one of the strongest bipartisan rebukes of Medicare home health cuts to date, the poll found overwhelming opposition across party lines. Large majorities of voters support targeting cost savings to eliminating waste and fraud rather than across-the-board cuts. Voters widely recognize that home health provides significant savings for taxpayers, that lack of access to home health due to recent cuts hurts Medicare patients, and that many more would be hurt if the proposed cuts go into effect.

“The results send a crystal-clear message: Americans want more home-based care, not less, and preserving access to care is critical. Cutting home health doesn’t save money – it hurts patients, worsens outcomes, and costs taxpayers more in the long run.”
The poll reveals Americans see home health as essential to keeping patients safe at home, lowering costs, and easing pressure on already overburdened hospitals and emergency rooms.
Key findings:
- 70% of all voters oppose Medicare cutting home health services by an additional 9% next year.
- 91% of all voters believe it’s important that home health services be available when Medicare patients require extra medical support.
- 55% of all voters support President Trump taking steps to reverse the proposed Medicare home health cuts and ordering a crackdown on fraud in the system.
- 71% of all voters believe home care is the most affordable care option, compared to just 17% who believe hospital care is more affordable.
- 73% of all voters say that cutting Medicare home health harms patients and legitimate providers while failing to stop the fraudulent operators that scam hundreds of millions of dollars from the program each year is a good reason to oppose the cuts.
“With more than one out of every two voters either on Medicare, or with a parent on Medicare, voters are clear that people want treatment at home if it’s an option and that home medical care is less expensive than care provided at hospitals and nursing homes. Voters also see the folly in across-the-board cuts that harm everyone rather than focusing efforts to root out known fraud in the home health system. Across the political spectrum voters oppose cuts and support redoubling efforts to fight fraud.”
“These numbers should give every lawmaker pause,” Dr. Landers cautioned. “Patients want to recover where they’re safest – at home. It’s time for Congress to protect what’s working and stop the home-care bleeding. Lawmakers have an opportunity to protect a program that saves lives, lowers costs, enjoys overwhelming bipartisan support, and reflects the clear will of the American people.”
The Alliance is urging Congress and CMS not to finalize the proposed payment cuts and to work with providers to revise their approach and strengthen, not weaken, access to home-based care.
A memo of the poll findings can be found here.
###
About the National Alliance for Care at Home
The National Alliance for Care at Home (the Alliance) is the leading authority in transforming care in the home. As an inclusive thought leader, advocate, educator, and convener, we serve as the unifying voice for providers and recipients of home care, home health, hospice, palliative care, and Medicaid home and community-based services throughout all stages of life. Learn more at www.AllianceForCareAtHome.org.