Meet the CMS Administrator Nominee
by Tim Rowan, Editor Emeritus
Mehmet Oz, MD, MBA is the CMS Administrator nominee in the new administration that assumes power on January 20. A popular TV personality and former gubernatorial candidate, the public side of Dr. Oz is well known, but the details of his life and his qualifications to head a $1.16 trillion government program less so. We reached out to the nominee’s PR firm on November 22 to request an interview but have not received a response. We gathered the following background information from his web site and other sources.
Heritage and Education
Mehmet Cengiz Öz was born on June 11, 1960 in Cleveland, Ohio, of Turkish immigrant parents. Raised in Wilmington, Delaware, he holds dual U.S. and Turkish citizenship and comes from healthcare roots. His father, Mustafa Oz, graduated at the top of his class at Cerrahpaşa Medical School in 1950 and moved to the United States to join the general residency program at Case Western Reserve University in Cleveland, where Mehmet was born. His mother, Suna Atabay, was the daughter of an Istanbul pharmacist.
Mehmet graduated with a biology degree from Harvard University in 1982. He earned an MD at the University of Pennsylvania School of Medicine and an MBA from Penn’s Wharton Business School in 1986. He completed his surgical training at NewYork-Presbyterian Hospital and served as a professor of surgery at Columbia University.
Completing his general surgery residency and cardiothoracic fellowship at Columbia-Presbyterian Medical Center in New York City, Oz became an attending surgeon at NewYork-Presbyterian Hospital/Columbia University Medical Center in 1993. He was later appointed professor of surgery at Columbia University in 2001. An advocate for integrating alternative medicine with conventional practices, he co-founded the Cardiac Complementary Care Center in 1995.
During his time at New York-Presbyterian, Oz patented the Mitraclip, a small implantable clip that can be placed using a catheter to repair the heart’s mitral valve. Oz reported earning over $333,000 in royalties from that product in his 2022 disclosures.
Rise to Fame
Oz gained national attention through appearances on “The Oprah Winfrey Show.” Winfrey’s production company, Harpo Productions, and Sony Pictures produced the daytime syndicated program, “The Dr. Oz Show,” which debuted in 2009. It won 10 Emmy Awards during its run.
The program, which focused on health and wellness topics, aired until 2022, when he left it to run for the U.S. Senate in Pennsylvania, winning the Republican nomination and eventually losing to Democrat John Fetterman. Oz is also a prolific author, with eight of his books on the New York Times bestselling list. The Dr. Oz Show gained in popularity during its run but occasionally faced criticism for promoting unproven health products and practices.
Finances
Most of what can be learned about Oz’s personal finances comes from disclosures he made during his Senatorial campaign. He reported a salary of $2 million as host of The Dr. Oz Show and $7 million from his stake in Oz Media. He was also paid $268,000 as a guest host on Jeopardy in 2021. In addition to salaries, Oz and his wife, Lisa, reported investments in big tech, health care, private equity funds, and various real estate holdings.
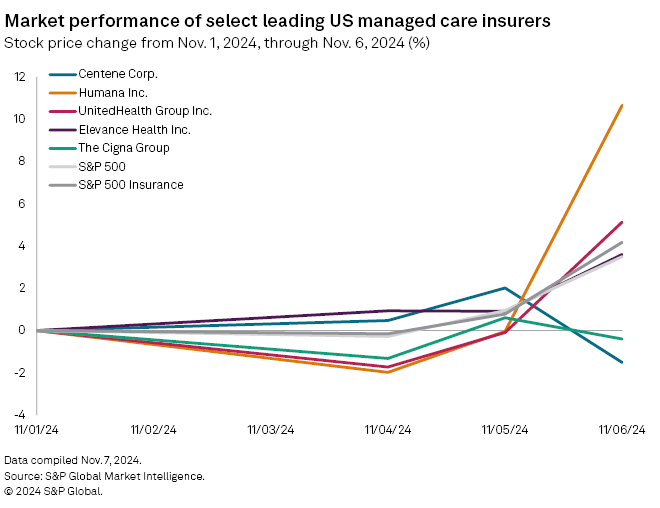
Oz’s 2022 financial disclosures showed Amazon stock worth up to $25 million; Microsoft, Apple, and Alphabet (Google) stock, each valued up to $5 million, and Nvidia stock valued up to $1 million. He also owned stock in UnitedHealth Group worth up to $500,000, and in CVS Health (Aetna), valued at up to $100,000. They also owned shares in privately owned gas station and convenience store chain Wawa valued between $5 million and $25 million. His 2022 disclosures showed he earned $5 million in dividends from his investment in Wawa.
The Oz’s also reported a real estate portfolio that includes residential and investment properties in New Jersey, New York, Pennsylvania, Florida, Maine, and his parents’ native country, Turkey, each valued from $1 million to $25 million. His 2022 disclosures also showed an investment property in Palm Beach and a cattle farm in Okeechobee, Florida, worth up to $5 million each, and $500,000 worth of cattle.
In addition to these investments, Oz currently runs the non-profit organization HealthCorps, which trains teenagers to share the organization’s curriculum on mental health, physical health, and nutrition. He also serves as Global Advisor and Stakeholder at iHerb, a company that sells supplements, personal care, grocery, and beauty products.
What Kind of CMS Would Oz Create?
What we know of Dr. Oz’s opinions regarding Medicare and Medicaid we learned from his 2022 Pennsylvania campaign message. During that campaign, Oz was a vocal supporter of privatizing Medicare. In 2020, Oz co-wrote an opinion piece in Forbes, suggesting “an affordable 20% payroll tax” to fund a “Medicare Advantage For All” program that could replace private insurance.
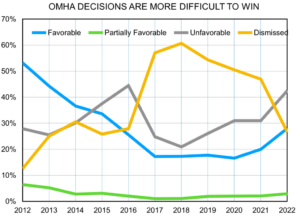
His plan, co-authored with Steve Forbes, suggested a 20% payroll tax, half paid by the employer, which the government would use to purchase a Medicare Advantage plan for everyone. The proposal did not explain how this would replace private insurance as MA plans are administered by insurance companies. Of course, this was four years ago, before it was widely known that MA plans pad patient assessments and deny care at a higher rate than straight Medicare does.*
CMS Administrator Nominee Outlook
Uncertainties to keep watch over include the CMS Administrator’s supervision over Medicaid and negotiating Medicare drug prices. If confirmed by the Senate, Oz would have the power to approve states’ requests to change their Medicaid plans, such as adding work requirements for beneficiaries.
He will also oversee drug price negotiations. The Inflation Reduction Act gave CMS the power to negotiate with pharmaceutical marketers to reduce the price of popular medications for people covered by Medicare Part D. The first round of negotiations concluded in August, and the next slate of drugs up for negotiations will be announced in February.
In nominating Dr. Oz, the President-elect said Oz will “help cut waste and fraud.” Whether that goal or seeing to the health of the more than a third of Americans insured through CMS programs becomes Mehmet Oz’s priority should be the first question asked in his Senate confirmation hearings.
Statement from National Alliance for Care at Home
I congratulate Dr. Oz on his nomination for CMA Administrator, I believe it generally is a good thing for patient care when physicians engage in public service and public policy leadership. I am still learning about his priorities and approaches for CMS and am looking forward to speaking with him about the importance of a vibrant and growing care at home sector. Home care and hospice offers CMS the greatest win-win opportunity in American healthcare; people get the independence and dignity they want and deserve while the taxpayers and families save on the costs of unnecessary hospitalization and institutionalization.
# # #

Tim Rowan is a 31-year home care technology consultant who co-founded and served as Editor and principal writer of this publication for 25 years. He continues to occasionally contribute news and analysis articles under The Rowan Report’s new ownership. He also continues to work part-time as a Home Care recruiting and retention consultant. More information: RowanResources.com
Tim@RowanResources.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com