by Rowan Report | Jun 13, 2024 | Artificial Intelligence, New Tech, Partner News
by Tom Herzog, COO of Netsmart
Navigating the Next Era of Tech-Enabled Healthcare
While the talk is about Artificial Intelligence, the immediate opportunity is Augmented Intelligence.
We are living through one of the most exhilarating times in healthcare, a journey made possible by significant milestones over recent decades. As healthcare technologists deeply committed to the cause + communities we serve, we’re excited by the promise of the upcoming era of technological empowerment. This phase is set to showcase and expand upon the extensive work done in digitizing healthcare, highlighting the relentless pursuit of innovation that has characterized our field. In conversations with colleagues and clients, we have recognized the need to explore these developments as we progress collectively. Matthew and I thought a series of reflections on these conversations would be helpful for all of us, providing insights into technology’s transformative impact on healthcare and the critical initiatives currently underway. We envision this dialogue as a series of posts throughout the year, sparking discussion and reflection as we navigate forward.
Back to the Future
In 2015, we envisioned a future where the concept of navigation as we know it would be obsolete, advocating for a universal search that is nearly autonomous, informed by the known context specific to every role. By 2019, we were discussing workflow automation, using the example of Lane Departure Warning systems in automobiles as a metaphor for technology that enhances outcomes through precision responses. The pace at which these technologies are evolving is astounding, moving beyond mere speed of thought to how we can iterate at the speed of innovation itself. Before we achieve the aspirations of true Artificial Intelligence, we must start with Augmented Intelligence, which may very well be the most significant technological innovation in my lifetime.
The Gentle Guidance of Technology: Augmented Intelligence in Healthcare
Artificial Intelligence (AI) and Augmented Intelligence stand as beacon forces driving innovation forward in this fast-evolving technology landscape. Drawing an analogy to driver assistance systems in modern vehicles, we explore the nuanced differences between these concepts, simplifying their understanding and underscoring the distinct roles in enhancing human capabilities.
Artificial Intelligence: The Autonomous Navigator
Imagine AI as the driving force behind fully autonomous vehicles, adeptly navigating complex terrains without human intervention. This epitomizes the grand aspiration of AI: to emulate or even transcend human Intelligence in specific tasks, thus granting machines the ability to function independently. It’s a prospect that is as exhilarating as it is intimidating, reminiscent of scenarios depicted in futuristic films. Such advancements bring to light profound questions about the limits of technology and the ethical considerations it entails. While we marvel at the potential, apprehension about the unknown shadows our enthusiasm. As we venture into this era, it’s imperative that we tread thoughtfully, balancing our ambitions with caution, as we unlock new realms of possibilities. Together, we must navigate this journey towards outcomes that are not only innovative but also meaningful and ethically sound.
Augmented Intelligence: The Co-Pilot’s Nudge
Conversely, Augmented Intelligence mirrors the driver assistance systems in vehicles – providing “nudges” or guidance while ensuring the driver remains in control. These systems bolster safety and efficiency, complementing human Intelligence with technological support. This partnership epitomizes the collaborative synergy between technology and human skills for a safer and more efficient driving experience.
The American Medical Association (AMA) aligns with this vision, emphasizing Augmented Intelligence’s role in enhancing human Intelligence rather than replacing it. The AMA advocates for the use of AI in healthcare as a means to augment the capabilities of medical professionals, not to substitute their critical thinking or clinical judgment.
Augmented Intelligence in Healthcare: Enhancing the User’s Ability
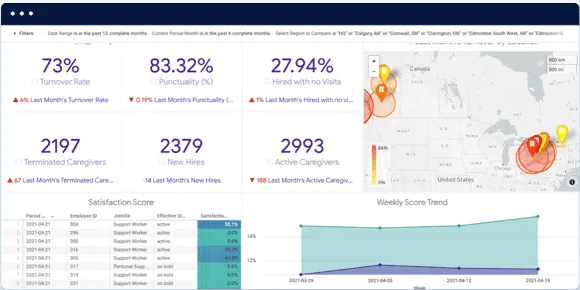
Reflecting on the transition from conceptual frameworks to tangible applications, we’ve initiated the Augmented Intelligence family. These solutions are meticulously designed to support clinical, operational, and financial workflows across all healthcare roles. Aimed at simplifying user experiences, these tools provide the best available context and automate information for validation and use as needed. This initiative marks a significant step in harnessing the potential of augmented Intelligence, enabling transformative shifts in healthcare practices and outcomes.
Michelle Donelan MP, reflecting on the U.K.’s commitment to AI in healthcare, highlights the transformative impact of augmented Intelligence, “AI will revolutionize the way we live, including our healthcare system. That is why we’re backing the U.K.’s fantastic innovators to save lives by boosting the frontline of our NHS and tackling the major health challenges of our time”. Donelan’s statement emphasizes the government’s support for utilizing AI to enhance healthcare delivery and address pressing health issues.
Augmented Intelligence promises to extend the partnership between human capabilities and technological advancement to medical professionals. Vincent Liu, MD, from Kaiser Permanente, elucidates this synergy, stating,
“There is a stage at which regulations can stifle some of the innovation [that AI might advance] … There is a role for providing a safe harbor [from certain regulations] so that we can use our best data to improve our patients’ care.”
This perspective underscores the potential of augmented Intelligence to enrich patient care by integrating comprehensive data analysis within the regulatory framework.
From the inception of conversations at our annual user conferences in the early 2000s to the present, we’ve witnessed the evolving landscape of healthcare technology. The decades-long journey of healthcare digitization has set the stage for today’s advancements, where Artificial Intelligence and Augmented Intelligence solutions leverage data to significantly improve care and operational efficiency.
Navigating Ethical Considerations
The integration of Augmented Intelligence in healthcare navigates through a maze of ethical considerations. Upholding the sanctity of the caregiver-patient relationship, ensuring patient privacy, and addressing potential biases in AI algorithms are paramount. The objective is to leverage Augmented Intelligence in a manner that respects these ethical boundaries while enhancing patient benefits.
A Future of Collaborative Care
Looking ahead, the promise of healthcare augmented by Intelligence offers a landscape where clinicians are equipped with unprecedented tools and information. This era does not diminish the essence of human judgment or the significance of the human touch in medicine but serves as a potent ally to these irreplaceable elements of care.
A Journey of Human-Machine Collaboration
Augmented Intelligence in healthcare symbolizes the collaboration between human Intelligence and artificial capabilities. This collaboration is not about relinquishing control but about enriching human expertise to tackle modern healthcare challenges. As we continue to integrate this technology, it heralds a future where healthcare is more personalized, predictive, and precise. The path forward, illuminated by the gentle guidance of Augmented Intelligence, promises a realm of endless potential for improved health outcomes for all.
Our immediate focus is three-fold 1) providing the communities we serve with the benefits of Augmented Intelligence, 2) ensuring we achieve Meaningful AI for every role, and 3) doing so through incremental progress so that AI now is a reality.
Final Thoughts
If you are reading this, you are likely one of the pioneers helping forge the path we are on today. If it were not for the initial efforts to digitize the ecosystem, we would not be talking about this today. Thank you for making this happen, for your perseverance and tenacity to find a way. Now we are at the transition from AI as a futuristic concept to its current role in shaping healthcare practices marks a remarkable chapter in the ongoing story of innovation in healthcare. It reaffirms the importance of digitization as the foundation upon which AI and other emerging technologies are built, enabling a future where healthcare is more informed, more empowered, and, ultimately, more human.
# # #
 Tom Herzog is responsible for leading solution and technology strategies focused on person-centric design to optimize workflow, efficiencies and outcomes. His teams work in collaboration with both clients and partners to deliver comprehensive solutions for the human services and post-acute care communities.
Tom Herzog is responsible for leading solution and technology strategies focused on person-centric design to optimize workflow, efficiencies and outcomes. His teams work in collaboration with both clients and partners to deliver comprehensive solutions for the human services and post-acute care communities.
Tom oversees multiple business units, including Netsmart consulting organization, solutions, development, engineering, technology, innovation, product development, IT, support, human resources, legal and operational functions.
Tom’s additional experience includes leading teams to automate systems and integrate financial, document management and information systems. He has been recognized for his ability to create innovative approaches and strategies that deliver results through vision and building strong teams.
Tom earned a bachelor’s degree in business management and human relations from Mid-America Nazarene University. He serves on the boards of the Overland Park Chamber of Commerce and the United Community Services of Johnson County.













 Tom Herzog is responsible for leading solution and technology strategies focused on person-centric design to optimize workflow, efficiencies and outcomes. His teams work in collaboration with both clients and partners to deliver comprehensive solutions for the human services and post-acute care communities.
Tom Herzog is responsible for leading solution and technology strategies focused on person-centric design to optimize workflow, efficiencies and outcomes. His teams work in collaboration with both clients and partners to deliver comprehensive solutions for the human services and post-acute care communities.