Medicare Prior Authorization
by Kristin Rowan, Editor
Medicare Prior Authorization
Wasteful and Inappropriate Service Reduction Model
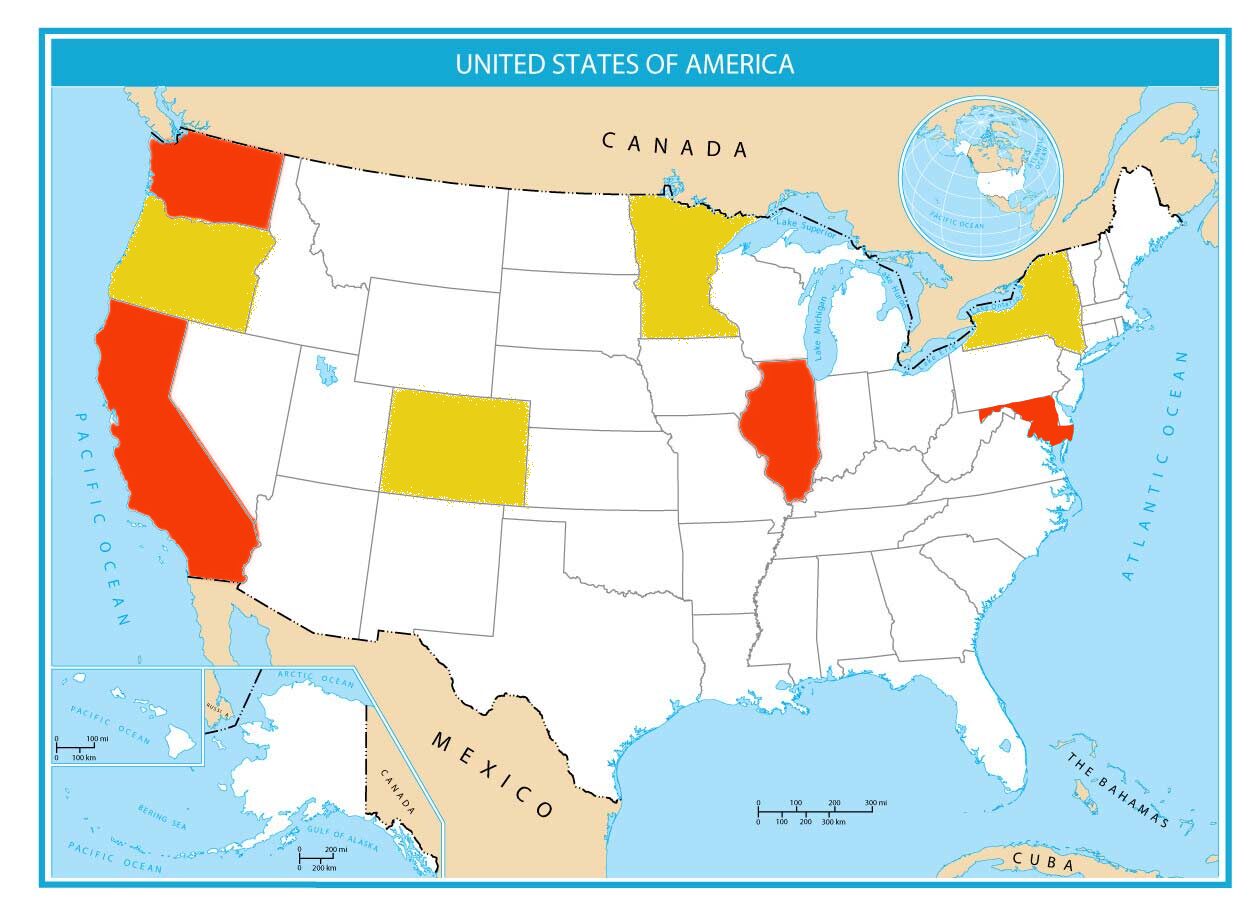
The Centers for Medicare and Medicaid Services (CMS) is launching a pilot program in six states to combat what they deem to be unnecessary treatments. Dubbed the Wasteful and Inappropriate Service Reduction (WISeR) Model, the voluntary program will launch in New Jersey, Ohio, Oklahoma, Texas, Arizona, and Washington beginning January 1, 2026 and ending December 31, 2031. The program will use Artificial Intelligence (AI) and Machine Learning (ML) alongside human clinical review to “ensure timely and appropriate Medicare payment for select items and services.”
The Problem
According to CMS, health care waste harms patients and comprises 25% of healthcare spending. “Low-value” services provide little effectiveness, do not align with specific health conditions, and can lead to additional complications and more wasteful services.
Medicare Prior Authorization Solution
The new WISeR Model is designed to reduce unsupported care. Participating care providers will outsource authorization of a pre-selected list of services to reviewers using technology to “expedite and improve the review process.” These services are those that CMS designated as vulberable to fraud, waste, and abuse.
Reasoning
CMS suggests that the fee-for-service model used in traditional Medicare incentivizes unnecessary treatments, tests, and other care. According to CMS, these items provide little to no benefit for some patients. These include:
- Skin and tissue substitutes
- Electrical nerve stimulator implants for obstructive sleep apnea and incontinence
- knee arthroscopy for knee osteoarthritis
- Cervical fusion
- Epidural steroid injections
- Vertebral augmentation
- Image-guided lumbar decompression
- deep brain stimulation for Parkinson’s and essential tremor
Strategy and Outcomes
The WISeR Model is supposed to ensure patients get the most appropriate care for the best outcomes. It is also supposed to lower costs and administrative burden on providers. Patients are supposed to partner with their health care providers to decide on the most appropriate care plan. Eliminating “unnecessary” services and procedures is supposed to save taxpayer dollars and decrease fraud, waste, and abuse. Care providers are supposed to focus on providing care that has the most impact on the well-being of Medicare beneficiaries.
Editorial Comment
I am not a Medicare recipient, but I have many close friends and family who are. I am not a nurse or home health expert, but I am a patient and by my count, I have a PCP and 6 specialists that I see on a regular basis. However, I am now, or will be in the near future, in need of:
- Electrical nerve stimulator
- Cervical fusion
- Steroid injections
- Lumbar decompression
Personal Experiences
I am already at the mercy of my health insurance provider for pre-authorizations for everything that is not routine visits with my primary care provider. I know first-hand the hoops and red tape my provider(s) go through. Already this year, I have filed two requests to review denials, more than 10 rescheduled visits because my pre-authorization had not been received, and at least one interview that my PCP had to attend with an “expert” who had previously decided that my regularly scheduled follow-up cancer scan was unnecessary.
Predicted Results
Adding prior authorization approval requirements for care and treatment will delay beneficiaries from getting the care they need, prolong the pain they experience daily, and cost more in wasted time and money than it can possibly save in wasted procedures. I sincerely hope there are enough voluntary participants in this experiment to document the additional time, money, and resources required. I also hope these participants send regular surveys to their Medicare beneficiaries to ask whether they feel like getting pre-authorizations for routine procedures has made them feel like they are getting better care.
# # #


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com