by Rowan Report | Feb 1, 2023 | Admin
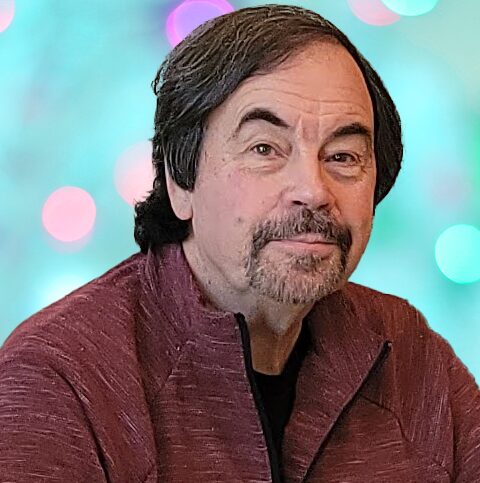
by Wendell Potter
Medicare Advantage is a money-making scam. I should know. I helped to sell it.
Right now, well-funded lobbyists from big health insurance companies are leading a campaign on Capitol Hill to get Members of Congress and Senators of both parties to sign on to a letter designed to put them on the record “expressing strong support” for the scam that is Medicare Advantage.
But here is the truth: Medicare Advantage is neither Medicare nor an advantage.
And I should know. I am a former health-care executive who helped develop PR and marketing schemes to sell these private insurance plans.
During my two decades in the industry, I was part of an annual collaborative effort to persuade lawmakers that Medicare Advantage was far superior to traditional Medicare — real Medicare. We knew that having Congressional support for Medicare Advantage was essential to ensuring ever-growing profits — at the expense of seniors and taxpayers. We even organized what we insiders derisively called “granny fly-ins.” We brought seniors enrolled in our Medicare replacement plans to Washington, equipped them with talking points, and had them fan out across Capitol Hill.
Instead of joining with the corporate lobbyists in extolling the benefits of Medicare Advantage while obscuring the program’s numerous problems… Congress should work to lower the cost of health care.
Apology and Accusation
I regret my participation in those efforts. Over the 20 years since Congress passed the Medicare Modernization Act, the Medicare Advantage program has become an enormous cash cow for insurers, in large part because of the way they have rigged the risk-scoring system to maximize profits. As Kaiser Health News reported last month, the Center for Medicare and Medicaid Services estimated “net overpayments to Medicare Advantage plans by unconfirmed medical diagnoses at $11.4 billion for 2022.” That was for just one year. Imagine what the cumulative historical total would be.
The Medicare and Medicaid programs have become so lucrative and profitable for insurers that UnitedHealth Group, the nation’s largest health insurer and the biggest in terms of Medicare Advantage enrollment, got 72 percent of its health plan revenues in 2021 from taxpayers and seniors. In fact, all of UnitedHealth’s enrollment growth since 2012 has been in government programs. Enrollment in the company’s employer and individual health plans shrank by 370,000 between September 30, 2012, and September 30, 2022. Much of the $81 billion UnitedHealth collected in revenues in the third quarter of last year was subsidized by American tax dollars.
Members of Congress on both sides of the political aisle – and both sides of the Capitol – are at long last calling for more scrutiny of the Medicare Advantage program. Sen. Chuck Grassley has called for aggressive oversight of Medicare Advantage plans to recoup overcharges and was quoted in the Kaiser Health News story. As was Sen. Sherrod Brown, who said that fixing Medicare Advantage is not a partisan issue. As Rep. Katie Porter commented, “When big insurance bills taxpayers for care it never intends to deliver, it is stealing our tax dollars.”
I know that Democrats and Republicans alike care about the financial stability of the Medicare program. Instead of joining with the corporate lobbyists in extolling the benefits of Medicare Advantage while obscuring the program’s numerous problems, and in the process helping Big Insurance make massive profits, Congress should work to lower the cost of health care.
Medicare Advantage is a money-making scam. I should know. I helped to sell it. And I am going to continue working alongside patients, caregivers, and elected officials to address the problems.
Wendell Potter is the former vice president for corporate communications at Cigna. He is now president of “Business for Medicare for All” and author of bestselling books Deadly Spin and Nation on the Take.
commondreams.org/author/wendell-potter
©2023 by Rowan Consulting Associates, Inc., Colorado Springs, CO. All rights reserved. This article originally appeared in Common Dreams.org. Reprinted by permission in Home Care Technology: The Rowan Report. homecaretechreport.com One copy may be printed for personal use; further reproduction by permission only. editor@homecaretechreport.com
by Tim Rowan | Feb 1, 2023 | CMS, Medicare Advantage, Regulatory
CMS Rule to Protect Medicare
The U.S. Department of Health and Human Services, through the Centers for Medicare & Medicaid Services, finalized the policies for the Medicare Advantage “Risk Adjustment Data Validation” program, which is CMS’s primary audit and oversight tool of MA program payments.
Under this program, CMS identifies improper risk adjustment payments made to Medicare Advantage Organizations in instances where medical diagnoses submitted for payment were not supported in the beneficiary’s medical record. The commonsense policies finalized in the RADV final rule (CMS-4185-F) will help CMS ensure that people with Medicare are able to access the benefits and services they need, including in Medicare Advantage, while responsibly protecting the fiscal sustainability of Medicare and aligning CMS’s oversight of both Traditional Medicare and MA programs.
As required by law, CMS’s payments to MAOs are adjusted based on the health status of enrollees, as determined through medical diagnoses reported by MAOs. Studies and audits done separately by CMS and the HHS Office of Inspector General have shown that Medicare Advantage enrollees’ medical records do not always support the diagnoses reported by MAOs, which leads to billions of dollars in overpayments to plans and increased costs to the Medicare program as well as taxpayers.
No Overpayments Collected Since 2007
“Protecting Medicare is one of my highest responsibilities as Secretary, and this commonsense rule is a critical accountability measure that strengthens the Medicare Advantage program. CMS has a responsibility to recover overpayments across all of its programs, and improper payments made to Medicare Advantage plans are no exception. For years, federal watchdogs and outside experts have identified the Medicare Advantage program as one of the top management and performance challenges facing HHS, and today we are taking long overdue steps to conduct audits and recoup funds. These steps will make Medicare and the Medicare Advantage program stronger.”
Secretary, Department of Health and Human Services
“CMS is committed to protecting people with Medicare and being a responsible steward of taxpayer dollars,” said CMS Administrator Chiquita Brooks-LaSure. “By establishing our approach to RADV audits through this regulation, we are protecting access to Medicare both now and for future generations. We have considered significant stakeholder feedback and developed a balanced approach to ensure appropriate oversight of the Medicare Advantage program that aligns with our oversight of Traditional Medicare.”
The RADV final rule reflects CMS’s consideration of extensive public comments and robust stakeholder engagement after the release of the 2018 Notice of Proposed Rulemaking. The finalized policies will also allow CMS to continue to focus its audits on those MAOs identified as being at the highest risk for improper payments. The RADV final rule can be accessed at the Federal Register.
Pre-Implementation Performance Report
The January 2023 Pre-Implementation Performance Report is now available to download from the Internet Quality Improvement Evaluation System (iQIES).
Instructions on how to access the PIPR are available below and on the Expanded HHVBP Model webpage under “Model Reports.”
To support home health agencies during this first performance year, CMS issued PIPRs in November 2022 and January 2023 to all active HHAs. The PIPR provides HHAs with data on their quality measure performance used in the expanded HHVBP Model, in comparison to HHAs nationally within peer cohorts, in advance of the first Interim Performance Reports (IPRs) in July 2023. The PIPRs do not contain calendar year (CY) 2023 data. The January 2023 PIPR includes a new tab containing preliminary achievement thresholds and benchmarks by volume-based cohort.
Need Help Understanding Your PIPR?
To assist HHAs in understanding the purpose, content, and use of the PIPRs, the HHVBP Technical Assistance Team created an on-demand video and downloadable resource, “Introduction to the Pre-Implementation Performance Report,” available on the Expanded HHVBP Model webpage. The video is also available on the Expanded HHVBP Model YouTube channel.
Additionally, the December 2022 edition of the “Expanded HHVBP Model Frequently Asked Questions” includes questions regarding the PIPR. If you do not see an answer to your specific question, please email the HHVBP Model Help Desk at HHVBPquestions@lewin.com.
If you experience an issue with accessing resources on the Expanded HHVBP Model webpage, first try refreshing the webpage. If that does not work, please try closing and reopening the browser. If you continue to experience issues, please try clearing the cache/cookies—links to instructions are below.
Locating the PIPR in iQIES
- Log into iQIES at iqies.cms.gov.
- Select the My Reports option from the Reports
- From the My Reports page, select the HHA Provider Preview Reports
- Select the HHVBP file to view the desired report. To quickly locate the most recently published report, select the down arrow adjacent to the Created Date label at the top of the table. This will order the reports in the folder from newest to oldest.
- Select the file name link and the contents of the file will display.
Should you experience difficulty locating the HHVBP file or with downloading, please contact the iQIES Help desk staff by email at
iQIES@cms.hhs.gov or by phone at (800) 339-9313.
For questions about the content of the expanded HHVBP Model reports, please contact the HHVBP Help Desk staff by email at HHVBPquestions@lewin.com.
*Please include your name, agency name, and the CCN when contacting the help desks.
Tim Rowan is a 30-year home care technology consultant who co-founded and served as Editor and principal writer of this publication for 25 years. He continues to occasionally contribute news and analysis articles under The Rowan Report’s new ownership. He also continues to work part-time as a Home Care recruiting and retention consultant. More information: RowanResources.com
Tim@RowanResources.com
©2023 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Tim Rowan | Sep 16, 2020 | CMS, Regulatory
Bi-Partisan Congressional Committees Demand CMS Administrator Repay Misspent Funds
his month, two House committees and two Senate committees published a report of a joint investigation into Centers for Medicare and Medicaid Services Administrator Seema Verma’s spending of taxpayer funds. The complete 56-page report is available in our “Partner News” section in the footer of our web site. For convenience, we reprint highlights from the report’s Executive Summary here.
The House Committee on Energy and Commerce, House Committee on Oversight and Reform, Senate Committee on Finance Minority, and Senate Committee on Health, Education, Labor, and Pensions Minority (the Committees) conducted a year-long investigation into Centers for Medicare & Medicaid Services (CMS) Administrator Seema Verma’s use of taxpayer funds to retain communications consultants with strong Republican political ties.
The Committees’ investigation shows that Administrator Verma and her top aides abused the federal contracting process to stock CMS with handpicked Republican consultants who billed the government hourly rates of up to $380. In less than two years, Administrator Verma’s consultants charged CMS nearly $6 million for work that included boosting her public profile and personal brand, serving as her preferred communications advisors, arranging private meetings for her with media personalities and other high-profile individuals, and routinely traveling with her to events across the country. By retaining these consultants, Administrator Verma misused funds appropriated by Congress, wasting taxpayer dollars intended to support federal health care programs.
The evidence obtained by the Committees expands on the findings of a recent audit conducted by the Department of Health and Human Services (HHS) Office of Inspector General (OIG) and demonstrates that Administrator Verma’s expenditures potentially exceeded the scope of CMS’s authority under the applicable appropriations. Congress appropriated taxpayer funds to CMS to ensure that Americans have access to and are aware of opportunities to enroll in federal health care programs, including Medicare, Medicaid, and the Affordable Care Act. Congress did not intend for Administrator Verma or other senior CMS officials to use taxpayer dollars to stockpile CMS with handpicked consultants or promote Administrator Verma’s public profile and personal brand. Given the reckless disregard she has shown for the public’s trust, Administrator Verma should reimburse the taxpayers for these inappropriate expenditures.
During the course of the investigation, the Committees obtained tens of thousands of pages of documents from HHS and private parties, conducted interviews and briefings with employees and executives from two of the consulting firms used by CMS, and collected additional information from databases, court records, and press reports, among other sources. The Committees’ investigation shows:
-
- Administrator Verma and her top aides misused federal contracts CMS held with consulting firms to bring handpicked Republican communications consultants into CMS operations.
-
- Administrator Verma and her top aides built a shadow operation that sidelined CMS’s Office of Communications in favor of the handpicked consultants.
-
- Consultants — particularly Pam Stevens — worked to promote Administrator Verma’s public profile and personal brand beyond her role as CMS Administrator, while also expanding the Administrator’s network.
- Administrator Verma’s consultants charged CMS nearly $6 million in less than two years.
-
- After CMS issued a stop-work order in April 2019, consulting firm Porter Novelli continued working for CMS under other task orders to pitch profile pieces on Administrator Verma to media outlets, including lifestyle magazines targeted in Pam Stevens’s Executive Visibility Proposal.
- OIG issued an audit on July 16, 2020 (OIG Audit) containing findings consistent with the Committees’ investigation and concluding that CMS violated federal contracting requirements. The OIG Audit, which was requested by the Committees, found:
-
- Administrator Verma and senior CMS officials allowed consultant Marcus Barlow to perform inherently governmental functions, such as making managerial decisions and directing CMS employees, thereby violating the Federal Acquisition Regulation (FAR).
-
- CMS improperly administered certain contracts it held with consulting firms as personal services contracts. In doing so, CMS officials exerted a level of control over the consultants’ work that created an improper employer-employee relationship, exceeding what was permissible under the contracts.
- CMS did not comply with the FAR and other federal requirements in managing contract deliverables, approving the use of a subcontractor, maintaining complete working files, and paying questionable
©2020 by Rowan Consulting Associates, Inc., Colorado Springs, CO. This article originally appeared in Home Care Technology: The Rowan Report. Click here to subscribe. It may be freely reproduced provided this copyright statement remains intact. editor@homecaretechreport.com
by Tim Rowan | Sep 9, 2020 | CMS
New Training, New HH Compare
Home Health Quality Reporting Training
September 01, 2020
Introduction to the Home Health Quality Reporting Program Web-Based Training
The Centers for Medicare & Medicaid Services is offering a web-based training course for those who are new to the Home Health Quality Reporting Program. This course is designed to provide a general overview of the program as well as a variety of links and resources for additional information. Specific topics include:
Lesson 1: What is the Home Health Quality Reporting Program (HH QRP)?
Lesson 2: The Outcome and Assessment Information Set (OASIS)
Lesson 3: OASIS Data Submission
Lesson 4: HH QRP Resources
CLICK HERE to access the training
Submit technical questions or feedback to: PAC Training mailbox.
Submit content-related questions to: HH Quality Reporting Program Help Desk
Home Health Compare merged with all other “Compare” databases
On September 3, CMS launched Care Compare, a streamlined redesign of eight existing CMS healthcare compare tools available on Medicare.gov. Care Compare provides a single user-friendly interface that patients and caregivers can use to make informed decisions about healthcare based on cost, quality of care, volume of services, and other data. With just one click, patients can find information that is easy to understand about doctors, hospitals, nursing homes, and other health care services instead of searching through multiple tools.
For more than 20 years, Medicare’s online compare tools have served as the cornerstone for publicizing quality care information for patients, caregivers, consumers, and the healthcare community. Today’s announcement builds on the eMedicare initiative that first launched by the Trump Administration in 2018 to deliver simple tools and information to current and future Medicare beneficiaries.
Drawing on lessons learned through research and stakeholder feedback, Care Compare includes features and functionalities that appeal to consumers. By offering a user-friendly interface and a simple design that is optimized for mobile and tablet use, it is easier than ever to find information that is important to patients when shopping for healthcare. Enhancements for mobile use will give practical benefits like accessing the tool using a smartphone can initiate phone calls to providers simply by clicking on the provider’s phone number.
Currently, someone who is planning to have bypass surgery would need to visit Hospital Compare, Nursing Home Compare, and Home Health Compare individually to research providers for the different phases of their surgery and rehabilitation. Now, those patients can start their search at Care Compare to find and compare providers that meet their healthcare needs that includes information about quality measures presented similarly and clearly across all provider types and care settings.
Patients will also find helpful hints and guides throughout Care Compare. For example, when searching for a nursing home, patients have the ability to utilize a checklist with common questions and considerations when selecting a nursing home. While the measures and data used for Care Compare have not changed, the way information is displayed is now different. During a transition period, consumers and other stakeholders will be able to use the original eight compare tools while CMS continues to gather feedback and considers additional improvements to the tool. As new information about quality and cost are added to the compare tools, Care Compare will be updated to reflect that information.
©2020 by Rowan Consulting Associates, Inc., Colorado Springs, CO. This article originally appeared in Home Care Technology: The Rowan Report. Click here to subscribe. It may be freely reproduced provided this copyright statement remains intact. editor@homecaretechreport.com
by Tim Rowan | Aug 19, 2020 | Clinical
New COVID Evidence Changes the Way Healthcare is Delivered
by Tim Rowan, Editor
In its August 12 edition, Smithsonian Magazine summarized new research conducted by epidemiologists and published both in The New England Journal of Medicine and a bulletin of the Centers for Disease Control and Prevention. What these scientists have discovered may have an impact on the way in-home clinicians, therapists, and other caregivers practice.
The report reveals findings that not only larger droplets but also microscopic aerosols can transmit the novel coronavirus that causes COVID-19. In fact, aerosols – measuring one-tenth the width of a human hair – can linger suspended in the air for hours. Droplets, which are expelled by sneezing or coughing, are much larger and fall to the ground or other surfaces much more quickly.
“While the difference is literally miniscule,” the report acknowledges, “knowledge of this route of transmission would result in significant changes in how the public can bring an end to the global pandemic. In the near term, it would inform social distancing and mask wearing recommendations from local governments, and in the long term, engineers and architects will need to rethink ventilation and air filtration in the design of everything from schools to cruise ships.”
Aerosols carry pathogens up to dozens of meters under the right conditions. How long a virus can remain airborne depends on the size of the droplet containing it. “That determines everything about how far it can travel, how long it can stay airborne before it falls to the ground,” says Linsey Marr, a professor of civil and environmental engineering at Virginia Tech.
While suspended in the air for hours, some experiments have shown it is possible for the aerosols to remain contagious “for many hours.” says Marr. Different experiments have produced widely varying results, from “more than an hour” in the NEJM report, to “up to 16 hours,” according to CDC researchers.
New discoveries underscore need for familiar prevention activities
- Hand-washing kills aerosols that are picked up while suspended in the air.
- Masks block aerosol sprays to varying degrees depending on the type of mask worn.
- Social distancing remains important because the concentration of aerosols is heaviest near an infected person.
The Smithsonian report concludes that airborne transmission of microscopic aerosols raises the issue of how to protect workers in healthcare settings. When PPE and respirators are in short supply, they should go to healthcare workers first. Surgical masks offer some protection, but it may not be enough for workers who routinely interact with the public. When an in-home care worker enters a patient’s home, they should be aware of the possibility of airborne aerosols and affix their mask well before someone answers the door. The cough that happened an hour before their arrival could be as dangerous as the one that happens while they are in the home.
Read the entire Smithsonian report here.
©2020 by Rowan Consulting Associates, Inc., Colorado Springs, CO. All rights reserved. This article originally appeared in Home Care Technology: The Rowan Report. homecaretechreport.com One copy may be printed for personal use; further reproduction by permission only. editor@homecaretechreport.com