by Kristin Rowan | May 10, 2024 | Admin, Caring for the Caregiver, Clinical, Regulatory
by Kristin Rowan, Editor
Last week, we reported on the proposed Bill in the Connecticut Senate and House to provide additional precautions for home care worker safety. In wake of the  Joyce Grayson murder during a home health visit, leadership in Connecticut aimed to safeguard home health and home health aide workers and collect risk assessment data on the same.
Joyce Grayson murder during a home health visit, leadership in Connecticut aimed to safeguard home health and home health aide workers and collect risk assessment data on the same.
On May 6, 2024, CT legislature passed bills in both the Senate and House of Representatives. Instead of the proposed bills that we reported on previously, both branches added amendments to previous bills. The bills include provisions for cyberattack readiness, child safety, and other items not related to care in the home.
First Stage of Home Care Worker Safety
Some of the provisions in the final bill are effective July 1, 2024. As we previously reported, hospice agencies are currently exempt from these provisions and the CT legislature will address hospice agencies in their next session.
On and after July 1, 2024
The Commissioner shall increase the fee payable to a home health care or home health aide agency that provides escorts for safety purposes to staff conducting a home visit to cover the costs of providing such escorts.
The Commission of Public Health will establish and administer a home care staff safety grant program to provide grants to home health and home health aide agencies for staff safety technology, including, but not limited to :
- A mobile application for staff to access safety information about a client
- A method for staff to communicate with either local police or other staff in the event of an emergency
- A global positioning system-enabled, wearable device that allows staff to contact local police
Effective July 1, 2024
The sum of one million dollars is appropriated to the Department of Public Health for the the fiscal year ending June 30, 2025, to establish and administer the aforementioned grant program.
The Commissioner of Public Health and the Commission on Community Gun Violence Intervention and Prevention, will develop or find educational material about gun safety practices and provide such to primary care providers to give to patients who are 18 years of age or older.
Second Stage of Home Care Worker Safety
Some of the provisions in the final bill are effective October 1, 2024. Home health and home health aide agencies have five months to comply with these measures.
Effective October 1, 2024, home health and home health aide agency must collect and provide to assigned workers information about:
The client, including as applicable;
- psychiatric history
- history of violence
- history of substance use
- history of domestic abuse
- current infections, if any, and treatment received
- whether diagnoses or symptoms have remained stable over time
Other persons present or anticipated to be present at the location of care including, if known to the agency:
- name and relationship to client
- psychiatric history
- history of violence or domestic abuse
- criminal record
- history of substance use
Location where employee will provide services including, if know to the agency:
- the crime rate for the municipality in which employee will provide services
- the presence of any hazardous materials, including, but not limited to used syringes
- the presence of firearms or other weapons
- the status and of the fire alarm system
- the presence of any safety hazards, including, but not limited to, electrical hazards
By October 1, 2024, each home health and home health aide agency must:
Provide staff training consistent with the health and safety training curriculum for home care workers, including but not limited to:
- Training to recognize hazards commonly encountered in home care workplaces
- Applying practical solutions to manage risks and improve safety
Conduct monthly safety assessments with each staff member and
Provide staff with a mechanism to perform safety checks, which may include, but need not be limited to:
- A mobile application that allows staff to access safety information about the client
- A means of communicating with local police or other staff in the event of an emergency
- A global positioning system-enabled, wearable device that allows staff to contact local police by pressing a button or through another mechanism
Effective October 1, 2024
Each home health and home health aide agency shall, in a manner prescribed by the Commissioner of Public Health:
- Report each instance of verbal abuse that is perceived as a threat or danger to the staff
- Report each instance of physical, sexual, or any other abuse by a client against a staff member
Third Stage of Home Care Worker Safety
No later than January 1, 2025
Beginning January 1, 2025 and annually therafter, the commissioner shall report to the joint standing committee:
- The number of reports of violence and abuse received
- The actions taken to ensure the safety of the staff member about whom the report was made
Effective January 1, 2025
Each individual health insurance policy shall provide coverage for escorts for the safety of home health care agency or home health aide agency staff
The joint standing committee of the General Assembly will convene a working group to study staff safety issues affecting home health and home health aide agencies, including but not limited to the following members:
- Three employees of a home health care or home health aide agency
- Two representatives of a home health care or home health aide agency
- One representative of a collective bargaining unit representing home health care or home health aide agency employees
- One representative of a mobile crisis response services provider
- One representative of an assertive community treatment team
- One representative of a police department; and
- One representative of an association of hospitals in the state
As we mentioned before, these regulations will become mandates across the country soon. OSHA has found the home care agency in Connecticut at fault for failing to implement safety procedures and precautions in the death of Joyce Grayson. The nurse’s family is suing the home health agency for wrongful death. Connecticut has established a protocol for safety measures, committees, reporting, and grant programs to implement immediate safety procedures across home health and home health aide agencies in the state. Before these provisions are passed on a national level, and before you have to tell the family of one of your staff that they aren’t coming home…
We urge you to:
- Create a safety committee within your agency
- Invest in training on de-escalation, workplace violence prevention, and self-defense
- Research and invest in a GPS-enabled emergency alert system for your staff. We recommend POM Safe and Katana Safety
- Insist on background information on all clients and others living in the home upon intake and BEFORE the first home visit
- Create a safe and comfortable way for your staff to report verbal abuse, violence, or uneasiness from any in-home visit
- Invest in escort and/or paired visits for high-risk clients, first-time clients, or any other situation that warrants it
We will continue to follow this story and provide updates as we receive them.
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Kristin Rowan | May 2, 2024 | Product Review
by Kristin Rowan, Editor
Revenue Cycle Management (RCM) addresses several pain points for care at home agencies: coding errors, timely reimbursement payments, and employee workload. Available as both full-service and SaaS products, RCM automation offers higher reimbursement rates, lower overhead costs, and overall better efficiency for your agency. Not having a RCM tool leaves your agency at higher risk for nonpayment, audits, and lengthy revenue cycles that impede your ability to manage your agency’s revenue.
Last week, I had the opportunity to talk with Michael Greenlee, Founder and CEO of HealthRev Partners. Hannah Vale, Chief Strategy Officer, joined him on the call. They told me about the HealthRev Partners’ launch of their new RCM tool, Velocity.
About HealthRev Partners
HealthRev Partners offers OASIS & POC Review and Coding assistance to home health, hospice, and palliative care agencies. The partnership program starts with an initial telephone conference, followed by a live review of documentation with an OASIS expert with recommendations for accuracy and compliance. Additionally, they have a precepting partnership program to enhance clinician performance and documentation practices. The RN guided program offers OASIS documentation review and correction sessions to ensure accurate and compliant documentation. Their solutions aim to maximize reimbursements with faster turnaround and higher accuracy.
HealthRev Partners Launches Velocity
On April 1, 2024, HealthRev Partners announced the launch of a new SaaS solution for Revenue Cycle Management, Velocity. HealthRev Partners designed Velocity to transform RCM for multi-site agencies. In addition to RCM, the tool offers operational insights for optimization and growth. Velocity focuses on real-time analytics and operational efficiency by centralizing data between locations. If you have an in-house RCM team, Velocity can be a stand-alone SaaS. However, if you need it, it can also be a full-service solution with outsourced coding and RCM experts on the Velocity team.
About Velocity
According to Michael Greenlee, many agencies lack tracking of their aging accounts receivable and the status of their claims. Without these, agencies can be leaving hundreds of thousands of dollars stuck in the revenue cycle without ever getting reimbursement from the claim. Velocity works with any existing EMR to pull data from coding and billing information. The built-in quality assurance (QA) solution is automated and customizable for charting and documentation. HealthRev Partners launched Velocity to help agencies overcome some of the pain points agencies have with RCM, billing, and coding.
Features
- Productivity and Accountability Reporting: Whether using Velocity as an outsourced solution or SaaS, instantly see time-stamped productivity reports, accuracy reports, and clinician QA scoring
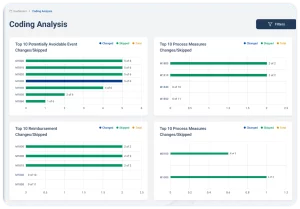
- Ai powered tracking: All claims in the 61-90 day and over 90 day segments are brought into the system for tracking with a follow-up reminder for each claim, payment information, and reasons for nonpayment.
- Claims forecasting: Velocity shows the current financial status of the agency, and with enough data in the system, can provide revenue forecasts simply by entering a future date into the reporting system.
- Pre-built database: All charting codes are built into the system and are searchable by keyword or phrase to reduce coding errors and increase reimbursement rates
- Platform agnostic: For many agencies, switching to a different EMR system costs more than the sticker price on the solution. With Velocity, there is no loss of data because it holds previous EMR data when you switch.
- Advanced Funding: Partners with Velocity have access to their AR funds before claims are processed, with an immediate credit line of up to $100,000, or 80% of the agencies AR.
Differentiation
Whether you need a software solution for your in-house RCM team or are looking to outsource your billing and coding to a partner, choosing the right RCM team is essential for your success. With so many RCM companies available in the market, it can be difficult to choose the right one. To choose the right RCM partner, there are a few factors to consider:
How does the solution or company match with the mission and vision I have for my agency?
HealthRev Partners has an “aspiration to develop innovative solutions that create boundless opportunities for our clients to advance their mission.”
Does the solution have the right tools for my success?
The analytics tools in Velocity can by customized to each agency’s KPIs. Velocity offers a fully supported software solution, a SaaS solution, and everything in-between to provide each agency with the level of support they need to succeed. Clinician productivity reports calculate clinician reimbursement by month. This shows which of your clinicians needs additional training and which should be recognized for their achievements, which can help to decrease your turnover rates. Velocity will custom build additional dashboards and measurements, included in the cost of the software.
Is the software solution safe for my agency and my clients?
Velocity is a HIPAA secure platform and is undergoing SOC-2 certification to protect your organization and the privacy of your patients.
Does the software partner have my best interests in mind?
Have you ever talked to someone who is so passionate about what they do that their energy is contagious? That was my experience in talking with Michael Greenlee, CEO and Founder of HealthRev Partners. Our one-hour scheduled software review meeting turned into a two hour conversation about what Velocity is designed to achieve. We also talked about how much potential it has to help home health, hospice, and palliative care agencies to survive.
Greenlee’s goal for Velocity is to have 0 claims go past 90 days for any agency they work with. They train each of their team members to meet the needs of an individual customer before they touch the account. HealthRev Partners offers “white glove service” to make good agencies great and to help partners dominate their marketplace. Michael partners with agencies he believes in as much as he believes in his own company. “We’re passionate about securing success for home health, hospice, and palliative care agencies across the nation.”
Future Considerations
Michael, Hannah, and I talked at length about what might be possible with Velocity. (So much so that Hannah asked if I was available to attend their next planning meeting.) AI capabilities are evolving and maturing at a rapid rate. Generative AI will become the standard for software solutions in care at home in short order. Michael’s passion for elevating the efficiency and prosperity of his home health, hospice, and palliative care agency partners will undoubtedly lead to even more innovation. Hannah Vale offered, “Our goal is to further enhance the sophistication of the AI. We consistently heed client feedback to creatively address their evolving requirements.”
To book a demo with HealthRev Partners, click here.
# # #
 Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. Additionally, she has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. Additionally, she has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Kristin Rowan | May 2, 2024 | Clinical, Regulatory
Home health agency failed to protect Joyce Grayson
History
We’ve been following the story of Joyce Grayson since her death in October of 2023. The news was first published in The Rowan Report here on November 8th, 2023.On April 14th, we reported on the pending Senate Bill in Connecticut that would require home health agencies to provide additional information and safety precautions prior to a home visit. The safety of solo workers is now even more important to home health and hospice agencies with the most recent update.
Today
May 1, 2024, the U.S. Department of Labor (DOL) posted a news release on their investigation into the death of Joyce Grayson, a home health nurse in Connecticut. According to the Department of Labor, OSHA has determined that Elara Caring exposed their employees to workplace violence from patients who were known to pose a risk to others. Jordan Health Care Inc. and New England Home Care Inc., both doing business as Elara Caring, have been cited for willful violation of the agency’s general duty clause. OSHA cited them for not developing and implementing safety measures to protect employees from workplace violence. They also cited the agency for failure to report work-related injury and illness records within four business hours.
Repercussions
OSHA has proposed more than $163,000 in penalties against Elara Caring. Elara Caring has 15 days from receipt of the citations to respond, request a hearing, or contest the findings.
“Elara Caring failed its legal duty to protect employees from workplace injury by not having effective measures in place to protect employees against a known hazard and it cost a worker her life,” said OSHA Area Director Charles D. McGrevy in Hartford, Connecticut. “For its employees’ well-being, Elara must develop, implement and maintain required safeguards such as a comprehensive workplace violence prevention program. Workplace safety is not a privilege; it is every worker’s right.”
OSHA found that Elara Caring could have reduced the potential for workplace violence by looking at the root causes of violent incidents and “near misses.” They could also have provided clinicians with background information on patients prior to a home visit. Other recommendations from OSHA include providing emergency panic alert buttons and using safety escorts for visits with high-risk patients.
Future Recommendations
The DOL states that employers should have a comprehensive workplace violence program. This program should include both management and employee involvement. Further, the DOL says this plan should have a written program with a committee. Elements of a workplace violence program include:
- Analysis of a home upon new patient admission
- Hazard prevention and control
- Training and Education
- Resources for Impacted Employees
- Recordkeeping
- Employee Feedback
Implications
If Elara Caring is fined for failure to keep their clinicians safe as a result of the investigation into Joyce Grayson’s murder, state and national level regulations are sure to follow. However, even if the laws in your area don’t change, investing now in workplace safety for your clinicians could save you from similar allegations and fines. As we mentioned in last week’s article about the Senate Bill, we have been in touch with several emergency alert companies and will be providing product reviews in the next few weeks. Start a workforce safety committee, develop a written plan for mitigating dangerous situations, and issue emergency response systems to all of your clinicians before it is your agency under investigation. More importantly, take these steps before your team loses one of its own to workplace violence.
# # #
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Kristin Rowan | Apr 26, 2024 | CMS, Recruitment & Retention, Regulatory
by Kristin Rowan, Editor
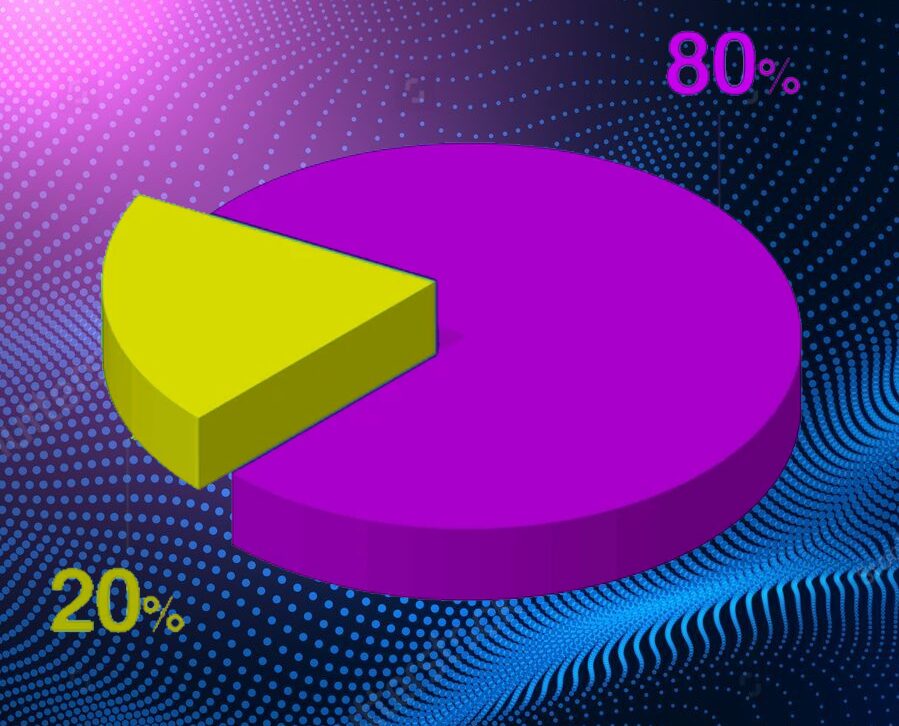
The Centers for Medicare and Medicaid Services (CMS) has finalized the “Ensuring Access to Medicaid Services” rule, more commonly known as the 80/20 rule. The 80/20 finalized rule requires at least 80% of Medicaid payments for home care services goes to caregiver wages. No more than 20% can be spent on administrative or other overhead costs. The White House, citing a study by The Commonwealth Fund, says that higher wages for caregivers will reduce turnover. Facing massive workforce shortages, home health, hospice, and supportive care at home agencies have been struggling to recruit and retain an adequate number of caregivers. The higher wage will also increase the quality of care, according to the study.
Prior to the 80/20 rule, there was no law or rule requiring home care agencies to report how they were spending money from federal medical payments. The rule includes requirements for states to create advisory groups to consult on rates and compensation. This changes the current Medical Care Advisory Committee regulations by increasing the percent of beneficiaries on the committee from 10% to 25% over the next two year. The Home Care Association of America (HCAOA) and the National Association for Home Care & Hospice (NAHC) argued that the rule adds administrative requirements to home care agencies while simultaneously reducing the resources available to fund them. NAHC President Bill Dombi said, “We all agree that more needs to be done to support the direct care workforce; however, this policy will make things worse, not better.” NAHC suggests the policy will force some agencies to close and others will leave the Medicaid program altogether, causing patients to have even more problems accessing care.
From the text of the final rule, CMS acknowledges additional comments that the minimum direct payment to caregivers in this rule will create hardships for some agencies. Across the country, there are substantial differences among waiver programs for HCBS that are not accounted for in the rule. There is some flexibility built into the rule to account for these factors, according to CMS. Some of the flexibilities include:
- Excluding some costs from the calculation
- Including clinical supervisors in the calculation
- Allowing states to set a different minimum for small providers
- Allowing states to develop their own criteria to qualify as a small provider
- Allowing states to develop criteria to exempt some providers from the rule
- Exemption from the minimum payment rule for all Indian Health Service and Tribal health programs
The final rule also changes the timeline for complying with the rule from four years after the date of publication to six.
Other comments included the need to address various reasons for the workforce shortage. In addition to low wages, commenters cited the social valuation of direct care work, lack of governmental support for some workforce pipelines, and immigration policies as deterrents to recruitment. One suggested that CMS start looking at creative strategies for developing an atypical workforce.
There were several submitted comments stating the either HHS or CMS or both does not have the authority under the Affordable Care Act to make specific requirements for minimum payments, but only to ensure that each State is assessing payment regulations and ensuring payments are economical, efficient, and ensure quality of care. A specific section of the Affordable Care Act, section 2402(a)(1) requires the Secretary of the Department of Health and Human Services (HHS) to ensure states implement service systems to allocate resources. The provision does not give HHS the authority to dictate the terms of those service systems, only to ensure the states develop those systems. Not surprisingly, CMS disagreed with those comments.
Many people questioned the 80% as being unrealistic, too high, and not based on quality data. CMS cited data from several states, who have pass-through requirements of 80-95% for all rate increases. This is not a minimum payment from all Medicaid payments, only a requirement for a minimum pass-through to direct care workers of increases in rates. Two states, Minnesota and Illinois, currently have minimum payment requirements set at 72% and 77%, respectively. CMS used these two states as justification for the 80% rule, acknowledging that it is higher than both states while also acknowledging that they did not perform a state-by-state study of the impact the 80% rule will have. CMS states the rate was set higher than those states to “encourage further steps towards improving compensation for workers.” CMS believes that requiring HCB agencies to pay their direct care workers a higher percentage of Medicaid rates than any state currently does will somehow make those agencies want to voluntarily pay even more.
The 80/20 Rule and Technology
Technological advances in telehealth, remote patient monitoring, revenue cycle management, scheduling, employee benefits, assistive technology, EVVs, EMRs, CRMs, and other software solutions can and will lower overhead costs and increase efficiency in your agency. Paperwork automation can reduce the time spent on documentation by a significant percentage. Revenue Cycle Management software can reduce claim denials and decrease reimbursement payment cycles so you can get your money faster. They can also reduce the number of unpaid claims. Employee benefit and training software can reduce responsibilities for HR teams, lessen the requirements for clinical supervisors, and cut training time in half, getting your newly recruited caregivers out in the field faster. Scheduling and onboarding software can increase your intake capabilities. The advances in generative AI allow you to create robust reports almost instantly so you can see your agency’s strengths and weaknesses and create plans for improvement.
Some of these costs will be excluded from the calculations for the 80% rule. Now is the time to invest in technology for your agency. Not only will your agency be more efficient and more effective, but you will be able to care for more patients with the same staff you have now, and the software solutions are as close to cost-neutral as they will ever be. We have a list of technology solutions that we’ve recently discovered and will be writing about in the next few weeks. If you are in immediate need of a software solution, contact us directly for a consultation.
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Kristin Rowan | Apr 18, 2024 | Vendor Watch
by Kristin Rowan, Editor
On February 21, 2024, HHAeXchange announced a change in leadership for the homecare management solutions company. Former Chief Revenue Officer Scott Schwartz was named Chief Operating Officer and new hire Lori Harrington came on board as the Senior Vice President of Product. You can read the press release from HHAeXchange here.
HHAeXchange provides management solutions for providers, MCOs, and state Medicaid agencies. The software was designed specifically for home and community-based services (HCBS) and connects state agences, MCOs, providers, and caregivers through its web-based platform. According to HHAeXchange, the personnel changes show the company’s “commitment to providing innovative solutions that some homecare industry challenges.
I had the opportunity to reach out to Scott and Lori to get, in their own words, their visions for the future of HHAeXchange and the industry.
The Rowan Report: Thank you, Scott and Lori for taking some time to talk with The Rowan Report. First, congratulations to you both on your new roles. Can you each share a little about your background and career?
Scott Schwartz: For over 20 years, I’ve focused on system of record, vertical SaaS software and technology, with experience leading sales, marketing, client success and operations. I started my career as a process engineer and have held leadership positions at several SaaS companies, including as the founder and general manager of CampSite. I joined HHAeXchange in 2017 as vice president and have also served as senior vice president and chief revenue officer before stepping into my current role. As chief operating officer, my aim is to galvanize the organization around a shared vision of operational efficiency, innovative service delivery, and customer satisfaction.
Lori Harrington: I have enjoyed a career of over 20 years in healthcare with a background in product strategy and informatics. In my most recent role as vice president of product management at Teledoc, I led product strategy for value-based care initiatives. My passion for digital transformation in B2B2C markets has driven successful healthcare initiatives from ideation to commercialization. I believe that success in healthcare is really understanding your users and building solutions to solve their everyday problems in a seamless, understandable way.
RR: Scott, as part of your new responsibilities at HHAeXchange, how will you ensure effective communication and collaboration between internal departments to better serve customers?
Scott: We’re focused on enhancing our platform, which connects state agencies, managed care organizations, providers and caregivers, so cross-departmental communication and collaboration are vital. With shared services such as implementation, revenue cycle operations, integrations, technical customer care, training, and customer education under my purview, I plan to streamline communication pathways and ensure all teams are aligned with and working toward our common goals.
We want to leverage our teams’ diverse talents to drive transformation. My approach includes fostering an integrated work environment where interdepartmental meetings, clear information channels, and shared objectives are the norm. Regular check-ins and transparent leadership are key to ensuring every department understands how their work directly benefits our clients, the members they serve, and the company’s broader goals.
RR: And how will you ensure HHAeXchange’s solutions and product enhancements meet the needs of all homecare stakeholders – caregivers, provider agencies, members, and payers?
Scott: Engaging with stakeholders is critical. We involve provider agencies, caregivers, payers and others in our development process to ensure that our platform addresses real-world needs effectively. Our comprehensive engagement strategies support this with initiatives like periodic customer summits, road shows, and information sessions to capture a wide array of insights and feedback.
We monitor industry trends, regulatory changes, and technological advancements, which are factored into planned enhancements and solution updates. And with a team of reputable industry experts, we’re working to ensure that our products exceed the evolving needs of all homecare stakeholders.
Lori: We understand that stakeholders in the homecare space have diverse and critical needs. We keep a pulse on industry trends and challenges such as issues with caregiver turnover, regulatory & compliance changes, increasing volume of live-in caregivers, and an increase in diversification in home care utilization. With these observations, we aim to provide products that support healthcare agencies and caregivers as these trends evolve. Our solutions must be built with a nimbleness that accounts for a continuous change in regulations, EVV compliance requirements, and stakeholder expectations. Frequently engaging with stakeholders, conducting thorough market research, and incorporating feedback loops are integral to our product development processes.
RR: Lori, you mentioned the diverse needs of your stakeholders. What are the greatest problems your clients and prospects say they are looking to solve with improved homecare management software solutions and EVV platforms?
Lori: Our clients are prioritizing caregiver retention and looking for comprehensive solutions to streamline operational processes like billing, HR, and payroll while ensuring regulatory compliance and providing high-quality member care. They need tools to manage the diverse locations of members’ and workers’ schedules, foster strong member-caregiver matches, and enable transparent communications among provider teams.
Taking those challenges into consideration, HHAeXchange aims to equip our solutions with time-saving, stress-reducing features. Operational worklists, for example, alert agencies to important dates and actions their teams need to take regarding caregiver compliance and client authorizations. Our appointment module and case broadcasting feature reduce hassles associated with scheduling visits and quickly filling unexpectedly open shifts.
RR: Two questions, Lori. What trends are you seeing that are transforming homecare delivery models and, in addition to technology, are there any other trends shaping the homecare industry in 2024?
Lori: The ongoing caregiver shortage remains a concern, driving a shift toward more strategic technology investments and training opportunities. Homecare delivery is becoming more person-centered, suggesting the industry has adjusted to EVV and is using the technology to incorporate collaboration with families as caregiver participants. Additionally, there’s a growing emphasis on self-direction, with clients seeking more choice, flexibility and control in their care. Compliance is gaining more attention, with increased scrutiny to ensure standards of care are met across the board. Data and analytics will continue to be a primary enabler for how healthcare is shaped. We account for all of this in our product strategy and development plans.
RR: Final questions for you, Scott. How does HHAeXchange envision the homecare industry evolving in 2024 and, more specifically, how do you see the company’s innovations playing a role in that transformation?
Scott: The homecare industry is at a critical juncture. As Lori said, we’ve noted significant shifts toward value-based care, self-directed care, and person-centered approaches. At the same time, the fundamentals of homecare are as important as ever. HHAeXchange’s role is to stay ahead of trends while improving product offerings and customer experiences. We strive to balance innovative thought leadership with steady progress, continually enhancing the functionality of our foundational platforms to meet clients’ needs.
We’re investing in scalable technology, service improvements, customer education, and strategic integrations to accommodate the industry’s evolution. Our leadership is committed to empowering providers and payers alike with tools to improve caregivers’ efficiency and address fraud, waste and abuse in the industry. Through these efforts and plans, we aim to facilitate a more sustainable, higher-quality, and accessible homecare ecosystem for all involved, ensuring members have the option to receive care and treatment in the comfort of their own homes.
RR: Thank you both, again, for your time. I wish you both great success in your new roles.
# # #
 Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Kristin Rowan | Apr 18, 2024 | Caring for the Caregiver, Clinical, Regulatory
In October of 2023, nurse Joyce Grayson went to the home (halfway house) of a released convict. She was later found dead in the basement of the house. In addition to adding focus to home care worker safety, the immediate response to this tragic event was an increase in nurses being afraid to do their jobs. Lawmakers in Connecticut vowed to increase protection for visiting nurses to ensure health care worker safety. The nurses requested additional reporting requirements for assaults while lawmakers suggested requiring an escort for high-risk situations.
Home Care Worker Safety by Law
Connecticut Senator Saud Anwar recognizes the growing segment of people wanting to age at home. “We want people to be able to get treatment at home,” he said. However, he also recognized the need for more information about potentially dangerous homes. He said at-home health care workers should be aware of what they’re walkin into “if there’s a high-risk situation.” Conn. lawmakers introduced Senate Bill One for Session Year 2024. The bill would require agencies to provide patient information, as applicable, including:
- Medical History
- Psychiatric history
- History of violence
- History of substance abuse
- History of domestic abuse,
- Current infections and treatments
- Stability of diagnoses or symptoms over time
- Housing Information
- Other persons in the home
- Name and relationship to patient
- Psychiatric history
- History of violence or domestic violence
- Criminal records
- History of substance abuse
- Location of Service
- Crime rate
- Presence of hazardous materials
- Presence of firearms or other weapons
- Status of location’s fire alarm system
- Presence of any other safety hazards
The bill also included ongoing safety training, safety assessments, and safety checks including:
- A mobile app with patient information
- A GPS enabled wearable device that allows staff to contact law enforcement
The Bill included payment rates to offset the cost of implementing all safety items to ensure cost-neutrality.
Implications for Hospice Agencies
Barbara Pearce, interim CEO of Connecticut Hospice, raised some legitimate concerns over the bill. Pearce warns that the background screenings required are lengthy and would result in many patients not receiving hospice care at all. According to Pearce, Connecticut Hospice “had 300 people die within three days, 200 people within two days, and 100 people within one day of entering home hospice care.” None of these patients would have been cared for if the bill had been in place at the time. Pearce discussed her concerns with Conn. lawmakers, who have since changed their approach.
Senate Bill One "Home Care Worker Safety" Moving Forward
Connecticut lawmakers are opting to exclude hospices from the bill for now. Sen Anwar said they plan to write a hospice-tailored bill “in the future” to ensure safety of hospice workers. Anwar continued, “We will have a plan of action to see what can be done to reduce the risk for hospice care workers too because…we want to make sure they’re safe too.”
The Connecticut 2024 legislative session is scheduled to adjourn on May 8. Senate and House representatives are racing the clock to modify the bill before the session ends.
Implication for Home Health
Few, if any, states have laws for home health worker safety. Alaska and Idaho have strict penalties for violence against health care workers. Wyoming introduced a similar bill in 2013, but it was defeated. Oregon passed a law in 2007 to require hospitals and surgery centers to implement safety strategies. Washington state established a law in 1999 that requires the development and implementation of a work-place violence plan. The law includes home health, hospice, and home care agencies, but does not have the detailed measures included in Connecticut’s bill.
If Senate Bill One passes in Connecticut, it could pave the way for additional state or federal regulations for in-home care safety precautions. Violence in home health, hospice, and home care has increased and steps need to be taken to ensure the safety and well-being of caregivers. Keep an eye out for some upcoming product reviews on mobile apps and hand-held emergency devices that allow home care workers to alert the agency, law enforcement, and/or family members before, during, and after a care visit.
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Kristin Rowan | Apr 11, 2024 | Admin, CMS, Regulatory
by Kristin Rowan, Editor
For a few weeks now, we have been covering the Change Healthcare cyberattack by ALPHV/BlackCat and the subsequent updates from CMS. Pharmacy and medical orders have been delayed, providers and patients are suffering, and CMS has issued “guidance” with no real solution. Underground reports indicate that Change Healthcare paid $22 million to BlackCat following the first cyberattack and that BlackCat stole 6TB of data from the system. Change Healthcare has refused to respond to questions about the alleged payment. Three weeks after the attack, Change Healthcare started to come back online, starting with the pharmacy services, which returned on March 7th. Parent company UnitedHealth Group indicated that other services would return in the coming weeks.
Legal Action
More than 87% of physicians are see more than a 20% drop in daily claim submissions. As of April 9th, physicians are still reporting issues with cash flow and anticipate higher than expected losses due to financing and loans that may be needed to cover them as the effects of the attack continue. Rivals of Change Healthcare are reportedly onboarding hundreds of customers who have left the organization. One of these, Availity, has processed more than $5 billion in claims that were left unprocessed by Change Healthcare’s system and has onboarded 300,000 providers with a backlog of more than 50 health systems waiting to start using the platform.
The attack has caused long-term disruptions, delays, cash flow problems, patient care disruptions, prescription delays, and billing issues. Some physician practices have started using personal money to cover payroll and other expenses. The US Department of Health and Human Services (HHS) has launched a formal inquiry into Change Healthcare’s data protection standards. This inquiry follows six class action lawsuits filed against the organizations. Physicians were still reporting significant impacts on their claims.
Adding Insult to Injury
Change Healthcare has barely gotten their systems up and running were still putting out fires when they were hit again.  On April 8, RansomHub contacted Change Healthcare and alleged to have 4TB of data stolen from the system and are demanding an extortion payment to keep the data private . RansomHub has threatened to sell the data, which includes US military personnel and patient data, medical records, and financial data, to the highest bidder in 12 days if the ransom isn’t paid.
On April 8, RansomHub contacted Change Healthcare and alleged to have 4TB of data stolen from the system and are demanding an extortion payment to keep the data private . RansomHub has threatened to sell the data, which includes US military personnel and patient data, medical records, and financial data, to the highest bidder in 12 days if the ransom isn’t paid.
Among the prevailing theories as to why Change Healthcare has been hit again is that the first ransom was supposed to have been split between ALPHV/BlackCat and an associate known as “notchy”, but ALPHV absconded with the ransom, leaving the other with nothing. Looking for a payout equal to what they lost, notchy partnered with RansomHub to try to recoup their losses. A second theory is that ALPHV and RansomHub are one in the same and that ALPHV went to ground after the ransom payout and have resurfaced as RansomHub. RansomHub, however, claims that after ALPHV went to ground, some of their affiliates joined the RansomHub operation and this is how they came by the data. Either way, it seems that the data stolen in the first attack was not returned after the ransom was paid and Change Healthcare is still susceptible to further extortion. This also means that the Change Healthcare system was not hacked a second time, but rather this is just an extension of the first data breach.
No word yet on whether Change Healthcare and UnitedHealth Group will pay the second ransom demand.
We will continue to follow this story and provide updates as it impacts payment and claims processing.
# # #

Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or
www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. www.therowanreport.com One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Kristin Rowan | Apr 4, 2024 | CMS, Regulatory
By Kristin Rowan, Editor
On March 28, CMS issued a new proposed rule to update Medicare hospice payments. Here’s what we know.
The new proposed rule:
- Would change the existing hospice wage index
- Clarifies current policy related to the hospice “eletion statement” and the “ntoice of election”
- Adds clarifying language around hospice certification
- Includes a request for information to get comments on implementing a separate payment mechanism for high-intensity palliative care services
- Proposes that Hospice Quality Reporting Program (HQRP) measures be collected through the Hospice Outcomes and Patient Evaluation (HOPE), adding two new measures
- Also proposes changes to the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Hospice Survey
The new proposed rule includes a net 2.6% increase in payments over FY 2024. This includes a 3% market-based update, and a 0.4% cut for productivity. Submitting quality data is a requirement of the net pay. Hospices that do not submit quality data will be penalized 4%, netting a 1.4% decrease in payments. The propsed rule for 2025 is .5% lower than the 2024 hospice payment increase.
The National Hospice and Palliative Care Organization (NHPCO) says the rate increase is good, but not high enough. NHPCO COO and Interim CEO, Ben Marcantonio said, “To continue providing the high level of care our patients and their families deserve, hospices require a payment rate that accurately reflects the current economic challenges. We know that hospice care has demonstrated $3.5 billion in annual savings for Medicare, which underscores the critical importance of investing in hospice to ensure continued beneficiary access to quality end-of-life care.”
Palliative Care
CMS is interested in feedback and proposals from hospice agencies for providing complex palliative treatments and high-intensity hospice care when that care negatively impacts hospices financially. CMS aims to care for high-cost patients through palliative care rather than acute care. The NHPCO agrees with the CMS proposal to fund palliative care separately from standard hospice or acute care. CMS will take feedback and proposals through May 28, 2024. Comments can be submitted electronically at http://www.regulations.gov, by following the “Submit a Comment” instructions. Comments can also be sent by regular or express mail. Addresses can be found in the full proposed rule. Follow the search instructions at http://www.regulations.gov to see all submitted comments.
The proposed rule can be viewed starting April 4, 2024 at the Federal Register at https://www.federalregister.gov/public-inspection.
# # #
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Kristin Rowan | Mar 28, 2024 | CMS, Regulatory, Uncategorized
By Kristin Rowan, Editor
Illumifin, an insurance administration and claims solution provider for long term care (LTC) insurance, has released its 2023 Cost of Care study. The longitudinal study is now in its tenth year and includes national, state, and regional costs of services across skilled nursing, adult day care, home health care, and assisted living facilities.
The study found that the average rate for a home health aide in 2023 was $30.62 per hour, a 5.2% increase over 2022. The average per-rate visit for a registered nurse was $147.72, a 1.6% decrease over the prior year. Assisted living facility rates are up .6 – 3.8% nationwide, while skilled nursing facility rates decreased .4 – 1.0%.
The full press release from Illumifin is here.
To access the full study, contact Jennifer Frost by email at jenniferfrost@illumifin.com.
As costs continue to rise, CMS will need to adjust its proposed per-episode base pay cut for FY 2025. We continue to report on the proposed cuts from CMS and MedPAC, who argue home health agencies are being overpaid, even as costs of supplies and hourly pay go up.
# # #

Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or
www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. www.therowanreport.com One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com
by Kristin Rowan | Mar 20, 2024 | CMS, Regulatory
By Kristin Rowan, Editor
In December, 2023, The Medicare Payment Advisory Committee (MedPAC) recommended a 22% payment reduction for hospice providers. This week, they’ve recommended additional cuts once again.
MedPAC has just released the March, 2024 Medicare Payment Policy Report, issued to Congress. The initial statement from MedPAC recognized the long-lasting impact of the COVID-19 pandemic on healthcare providers and the record inflation rates. The commission admits that the pandemic has caused burnout and personal risk to clinicians and other health care workers. The commission also admits that the effects of COVID-19, PHE-related policy changes, and emergency funding made it difficult to interpret the indicators of adequacy in Medicare’s payment rates.
The commission openly states that the fundamental problem with FFS Medicare payments is that providers are paid more when they deliver more services, whether or not those services provide value. The call for additional payment reforms to force providers to coordinate care over time and across care settings and to eliminate what may be necessary services that MedPAC doesn’t deem valuable.
Home Health Agencies
The commission reports the Medicare margins for HHAs at 22.2 percent in 2022. The commission calculates these margins excluding some fixed costs. The margins, according to the commission, indicate that FFS Medicare payments exceed the costs of care. This should incentivize HHAs to take on additional beneficiaries, as the margins are calculating using only costs that diminish by volume.
The commission notes a drop in HHA use in 2022 and lists possible causes including:
- The number of FFS Medicare beneficiaries is lower due to the increased enrollment in Medicare Advantage
- Lower use of inpatient hospital care among FFS beneficiaries
- Hospitalized FFS beneficiaries were less likely to be discharged to home health care (no reason for this was given)
- More FFA beneficiaries are using SNFs after hospitalization (no reason for this was given)
- The staffing shortages reported by HHAs limit the volume of services they can provide
The commission implies that the staffing shortages are not a factor in the decline in HHA usage. The Department of Commerce’s employment data indicates staffing levels that are currently higher than pre-pandemic levels. Even though the data includes HHAs, hospice, private duty, pediatric agencies, and other home care providers, the commission still contends that Medicare HHAs comprise a significant enough share of this group to conclude there is no staffing shortage nationwide.
The commission also reports that the decrease in the number of HHAs nationwide is not a factor in the decline of HHA usage, because most beneficiaries still live in an area with at least on HHA. The commission recognizes that the number of employees and contract laborers is not used to calculate access to care, even though it is a factor. They also admit that an HHA does not need to serve an entire area to be counted as serving the area, and that the capacity to serve additional beneficiaries is not considered.
The report recognizes that preventable readmissions to hospitals is lower among for-profit and free-standing HHAs than for hospital-based care. However, the commission dismisses this data in favor of the all-cause measure of hospitalization, which is much higher for HHAs. This measure covers 60 days and includes all hospitalizations for any cause and includes community-admitted and home health admitted patients. Essentially, MedPAC is assigning a 14.2 percent hospitalization rate to all home health patients, regardless of the cause of hospitalization, whether or not it is deemed preventable, and whether or not it is in any way related to the initial 30-day-period of post acute care.
The average cost of a 30-day period increased by 4 percent in 2022, due to a higher cost per visit. The HHAs are combatting this by reducing the number of in-person visits per 30-day period. Since MedPAC did not track telehealth visits, there is no data on the overall cost per visit, regardless of whether it was in person or remote. HHAs are working within the PDGM model for reimbursement by lowering their overall costs per 30-day period through telehealth visits, remote patient monitoring, and other technologies implemented to increase efficiency in HHAs. MedPAC wants to penalize this by reducing payment rates. This will only serve to push HHAs to further decrease the number of visits, which will impact quality of care, satisfactions rates, and rehospitalization rates.
The commission concludes that because the payments exceed the costs, the benefits of home health care are devalued as a substitute for more costly care options. MedPAC argues that the overpayment since 2000 creates higher expenditures for beneficiaries, but fails to provide data to this effect.
As noted by NAHC, there are flaws in MedPACs calculations as well as in the foundation of their position:
- Exclusions such as taxes, telehealth, and marketing in cost calculations incorrectly inflate the margins
- MedPAC relies heavily on the CMS calculations for budget-neutrality, which NAHC has already refuted as incorrect, bordering illegal formulas
- The data used in these calculations omitted all HHAs that are hospital-based.
NAHC, along with other agencies, will continue to advocate on behalf of HHAs, hospice providers, and other home-based care agencies in front of Congress to ensure these disastrous cuts will not become permanent inclusions in Medicare policy. We will continue to bring you updates as this issue continues to unfold.
# # #
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. She has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report.homecaretechreport.com One copy may be printed for personal use: further reproduction by permission only.
editor@homecaretechreport.com
 Joyce Grayson murder during a home health visit, leadership in Connecticut aimed to safeguard home health and home health aide workers and collect risk assessment data on the same.
Joyce Grayson murder during a home health visit, leadership in Connecticut aimed to safeguard home health and home health aide workers and collect risk assessment data on the same.




 Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. Additionally, she has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or
Kristin Rowan has been working at Healthcare at Home: The Rowan Report since 2008. She has a master’s degree in business administration and marketing and runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in event planning, sales, and marketing strategy. Additionally, she has recently taken on the role of Editor of The Rowan Report and will add her voice to current Home Care topics as well as marketing tips for home care agencies. Connect with Kristin directly kristin@girardmarketinggroup.com or 



 On April 8, RansomHub contacted Change Healthcare and alleged to have 4TB of data stolen from the system and are demanding an extortion payment to keep the data private . RansomHub has threatened to sell the data, which includes US military personnel and patient data, medical records, and financial data, to the highest bidder in 12 days if the ransom isn’t paid.
On April 8, RansomHub contacted Change Healthcare and alleged to have 4TB of data stolen from the system and are demanding an extortion payment to keep the data private . RansomHub has threatened to sell the data, which includes US military personnel and patient data, medical records, and financial data, to the highest bidder in 12 days if the ransom isn’t paid.


