Non-Compliance Notifications & HOPE Training
CMSby Kristin Rowan, Editor
Hospice Non-Compliance Notifications
On July 21, 2025, the CMS Hospice QRP Announcements page added an update titled “Hospice Quality Reporting Program: Non-Compliance Notifications.”
The Update Reads:
The Centers for Medicare & Medicaid Services (CMS) is providing notifications to hospices that were determined to be out of compliance with Hospice Quality Reporting Program (HQRP) requirements for calendar year (CY) 2024…. This will affect their fiscal year (FY) 2026 Annual Payment Update (APU). The Medicare Administrative Contractors (MACs) will distribute Non-compliance notifications and place them into hospices’ Certification and Survey Enhanced Reporting (CASPER) folders in QIES on July 21, 2025. Hospices that receive a letter of non-compliance may submit a request for reconsideration to CMS via email no later than 11:59 pm, August 26, 2025. If you receive a notice of non-compliance and would like to request a reconsideration, see the instructions in your notification and on the Reconsideration Requests webpage.
Details
Any reconsiderations containing protected health information (PHI) will not be processed. All PHI must be removed for a reconsideration to be reviewed.
Additionally, all submissions must be less than 20 MB overall (email message and attachments). Submissions that are greater than 20 MB in size cannot be processed.
HOPE Training
As the implementation date for the HOPE tool drew nearer, advocacy groups and hospice agencies expressed concern over it’s readiness. On June 6, 2025, The Rowan Report shared that three of the largest organizations urged CMS to delay the tool. The groups asked for proper information, education, and training.
CMS Response
As of now, CMS is not delaying the implementation of the HOPE tool. They have, however, published training tools for hospice providers. The first series of videos is Didactic Training. They cover an introduction to the tool, admin information, preferences and active diagnoses, health conditions, skin conditions, and medications.
On July 21, 2025, CMS announced the opening of registration for live HOPE training. “Hospice Outcomes and Patient Evaluation (HOPE) National Implementation Virtual Training Program Course 2: Coding Workshop.” CMS recommends completing The Didactic Training as a prerequisite to the Coding Workshop.
The Centers for Medicare & Medicaid Services (CMS) is offering a live coding workshop on August 5, 2025…. It will provide coding practice for items that are new for HOPE, as well as the existing and updated items carried over from the Hospice Item Set (HIS).
Register now at:The Hospice Outcomes and Patient Evaluation (HOPE) National Implementation Coding Workshop
Find the Didactic Recorded Training Series here.
Data Collection Starts Soon
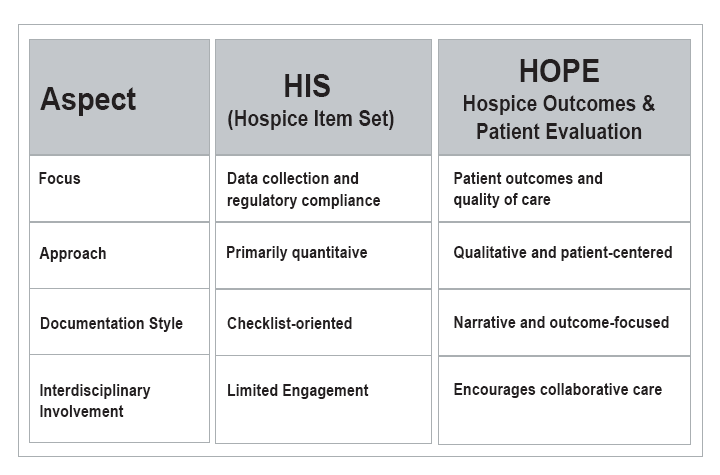
The HOPE tool begins data collection on October 1, 2025. Key items hospice providers should understand:
- More Frequent Assessments: HOPE introduces up to four assessment points per patient, capturing care from multiple angles during the first 30 days and at discharge.
- Real-Time Data Capture: Unlike the retrospective nature of HIS, HOPE assessments are completed during live patient encounters, providing richer and more immediate insights.
- Higher Stakes for Compliance: To avoid a reimbursement cut of up to 4%, agencies must ensure that at least 90% of HOPE assessments are submitted on time—a notable increase from the previous 2% penalty under HIS.
- Public Reporting Timeline: While HIS data has been publicly available, HOPE data will not be released for public comparison until fiscal year 2028 or later, giving providers time to adapt.
*from the SimiTree blog: Understanding the Transition from HIS to HOPE
As the implementation of the HOPE tool gets closer, we will continue to share training information from CMS and other sources as it becomes available. If you need a referral to a hospice consultant to navigate the transition, please reach out to The Rowan Report.
# # #


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com



 Earl L. “Buddy” Carter is an experienced businessman, health care professional and faithful public servant. For over 32 years Buddy owned Carter’s Pharmacy, Inc. where South Georgians trusted him with their most valuable assets: their health, lives and families. While running his business, he learned how to balance a budget and create jobs. He also saw firsthand the devastating impacts of government overregulation which drives his commitment to ensuring that the federal government creates policies to empower business instead of increasing burdens on America’s job creators.
Earl L. “Buddy” Carter is an experienced businessman, health care professional and faithful public servant. For over 32 years Buddy owned Carter’s Pharmacy, Inc. where South Georgians trusted him with their most valuable assets: their health, lives and families. While running his business, he learned how to balance a budget and create jobs. He also saw firsthand the devastating impacts of government overregulation which drives his commitment to ensuring that the federal government creates policies to empower business instead of increasing burdens on America’s job creators. Congressman Ami Bera, M.D. has represented Sacramento County in the U.S. House of Representatives since 2013. The 6th Congressional District is located just east and north of California’s capitol city, Sacramento, and lies entirely within
Congressman Ami Bera, M.D. has represented Sacramento County in the U.S. House of Representatives since 2013. The 6th Congressional District is located just east and north of California’s capitol city, Sacramento, and lies entirely within