First Joint Event for NAHC & NHPCO
FOR IMMEDIATE RELEASE
July 30, 2025
PHOTO LINK
National Alliance for Care at Home Hosts Inaugural Financial Summit
Over 700 industry leaders gather in Chicago for three-day event focused on financial leadership and innovation in home-based care
(Alexandria, VA and Washington, DC) — The National Alliance for Care at Home (the Alliance) successfully hosted its inaugural event, the 2025 Alliance Financial Summit, July 27-29 in Chicago, IL. The Summit brought together financial leaders from across the care at home community, with expert-led sessions, peer collaboration, and insights into market shifts and emerging technologies.
Arrival in Chicago
Welcome
The Summit officially launched Sunday evening with an opening keynote by Wendy Sue Swanson, MD, MBE, Founder and CEO of Skin Metal and Author of “Mama Doc Medicine.” Dr. Swanson delivered a forward-looking presentation on the intersection of medicine and technological innovation. The evening concluded with a Welcome Reception in the Exhibit Hall.
Keynote
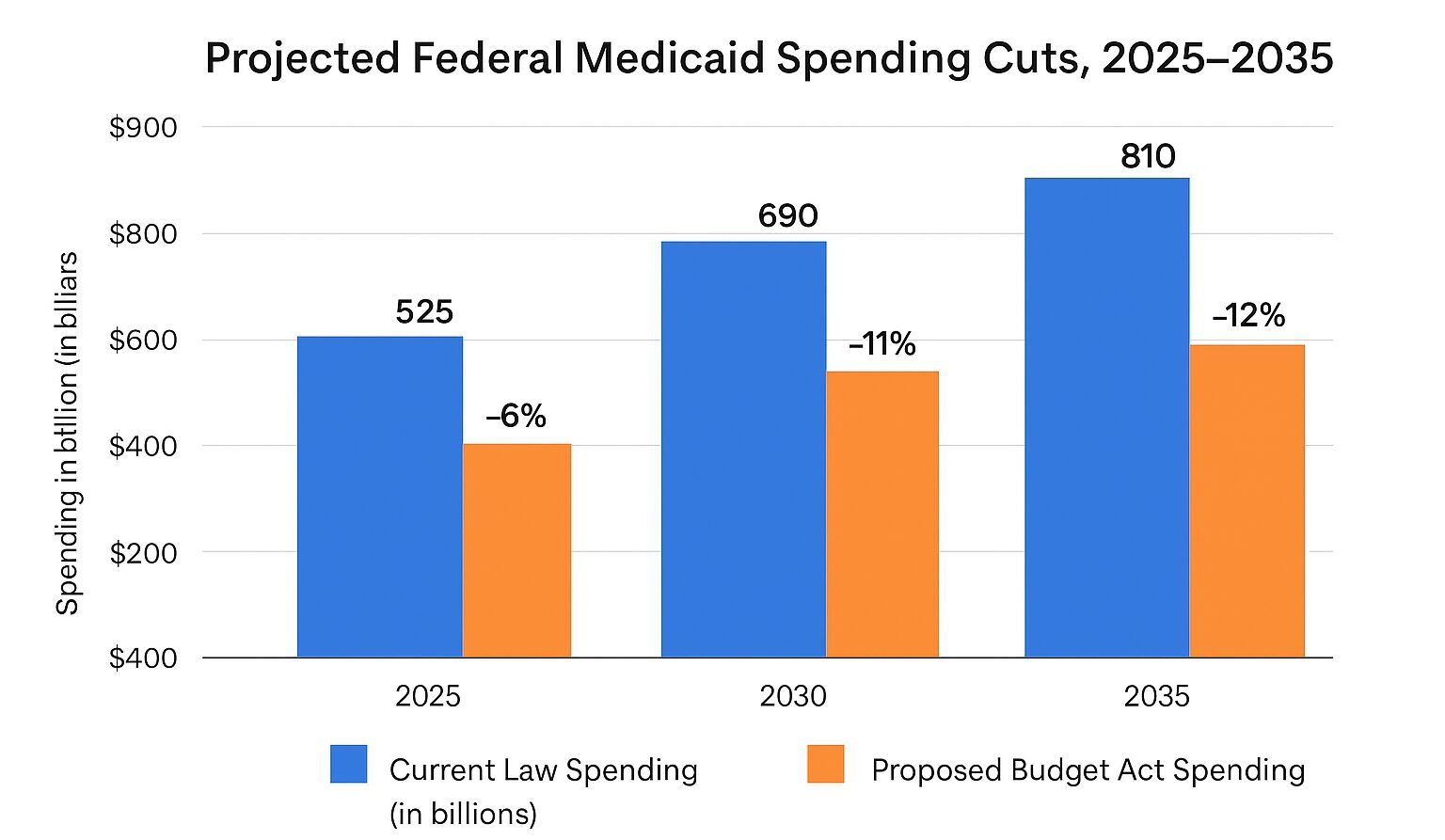
The day’s keynote session featured Alliance CEO Dr. Steve Landers alongside a panel of experts including Ken Albert, President and CEO of Andwell Health; Trisha Crissman, President and CEO of CommonSpirit Health at Home; and Hillary Loeffler, Vice President of Policy & Regulatory Affairs for the Alliance. Panel discussions addressed the potential impact of payment cuts in the Centers for Medicare & Medicaid Services Calendar Year 2026 Home Health proposed rule, hospice policy developments, workforce challenges and solutions, and actionable strategies for providers to protect the future of home-based care. Attendees then moved into a full day of concurrent sessions before an evening reception on the Chicago River.




Networking and Education
Tuesday featured dedicated peer-to-peer networking sessions, allowing for informal conversation and knowledge sharing, before the opportunity for more concurrent sessions. The Summit concluded with a closing keynote expert panel featuring leaders from the Alliance’s Home Health and Hospice Financial Managers Association (HHFMA).
“This first Alliance event exceeded our expectations, bringing together care at home leaders from across the nation to connect, learn, and recommit to our shared vision of an America where everyone has access to the highest quality, person-centered healthcare wherever they call home,” said Alliance CEO Dr. Steve Landers. “The content was both practical, grounded in the day-to-day challenges and successes of providers, while incorporating innovation and aspiration to drive future growth and success.”
The Alliance has announced two additional events for 2025: Alliance Advocacy Week, September 8-11 in Washington, DC, and the National Alliance for Care at Home Annual Meeting and Exposition, November 1-4 in New Orleans, LA.
# # #
About the National Alliance for Care at Home
The National Alliance for Care at Home (the Alliance) is the leading authority in transforming care in the home. As an inclusive thought leader, advocate, educator, and convener, we serve as the unifying voice for providers and recipients of home care, home health, hospice, palliative care, and Medicaid home and community-based services throughout all stages of life. Learn more at www.AllianceForCareAtHome.org.
Press Contact
communications@allianceforcareathome.org
Elyssa Katz | 571-281-0220