CMS Proposed Changes
by Kristin Rowan, Editor
CMS is Making Changes
Good or Bad?
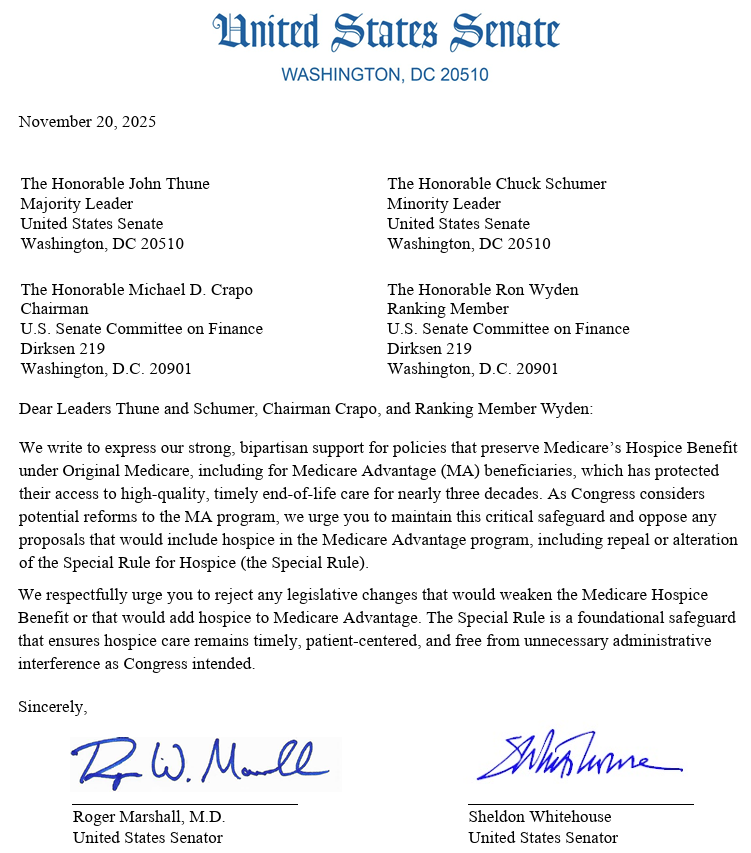
CMS is making changes across Medicare and Medicare Advantage. From Star Ratings to Prescription Drug Prices to the Hospice benefit, CMS is embracing Make America Healthy Again. Will these initiatives benefit Medicare and Medicare Advantage recipients or the insurance companies who provide the plans?
Drug Payment Model
In early November, CMS announced a plan to lower prescription drug costs for Medicaid recipients. State Medicaid programs can opt in to the GENErating cost Reductions fOr U.S. Medicaid Model (GENEROUS). The pilot program is using the most-favored-nation pricing that was recently negotiated and announced by President Trump. Most-favored-nation pricing requires prescription drug manufacturers to charge the same low rate paid in other countries.
Limited Pilot
Beginning in 2026, CMS will negotiate with manufacturers of select drugs for lower pricing. Participating states will start using uniform, transparent coverage criteria. This is not criteria for inital coverage in Medicaid, but for standardizing access to high-cost medications.
Manufacturers are not required to participate in the GENEROUS Model, but can voluntarily apply. Participating manufacturers agree NOT to seek additional supplemental rebates or discounts outside the model price.
New Medicare Advantage Policies
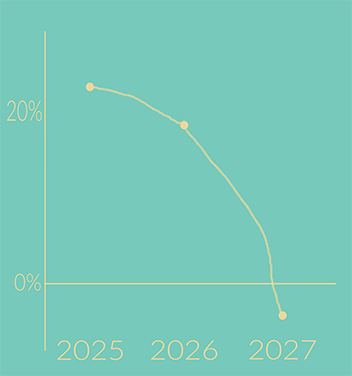
CMS has proposed updates to the Medicare Advantage and Medicare Part D programs. The new plan would begin in CY 2027 and includes major changes to the Star Ratings system. CMS is also seeking feedback on new ways to modernize MA.
Star Rating Changes
The proposed changes are supposed to incentivize plans to improve care. CMS suggests removing 12 unique measures that look at administrative processes and those that don’t highlight differences between plans. Star Rating measurements of care, outcomes, and patient experience will remain.
Request for Feedback
CMS is seeking feedback on Medicare Advantage changes, including improving competition, refining risk adjustment, and aligning quality incentives to deliver greater value. CMS is open to either a limited model test or program-wide changes. Interested parties can submit feedback through January 26, 2026. Read the Proposed Rule here. Submit your comments.
Expanding Technology-Enabled Care
CMS may finally be recognizing what we’ve been promoting for 25 years: Care improves with technology support.

The ACCESS model tests a new payment approach in original Medicare to expand access to technology-supported care options. CMS aims to increase technology-supported care options to improve health and prevent and manage chronic diseases. More than two-thirds of Medicare beneficiaries are dealing with high blood pressure, diabetes, chronic musculoskeletal pain, and depression.
An interest form is now available for the 10-year Advancing Chronic Care with Effective, Scalable Solutions (ACCESS) Model test. The model test begins July 1, 2026. The application to participate must be received by April 1, 2026.
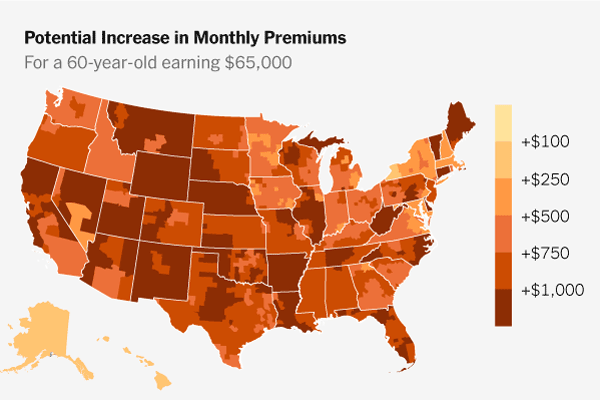
Impact
As these programs roll out between now and 2029, the impact on insurance plans, payors, beneficiaries, and taxpayers will unfold. Will lower cost prescriptions and technology-based care lower insurance rates? Payor reform may be necessary to change out-of-pocket costs. Regulations may have to further incentivize payors to increase care when costs go down, particularly with value-based care models.
Please take a few minutes to read the details on each of these proposals, add your comments, and sign up to participate. The industry needs reform and our aging family members deserve better.
# # #


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com