Dr. Steve Landers: an Interview
by Kristin Rowan, Editor
Dr. Steve Landers
An Interview from the Alliance Annual Meeting
On the heels of the inaugural National Alliance for Care at Home Annual Meeting & Expo, I sat down with Alliance CEO Dr. Steve Landers to talk about his feelings on the event, the current state of the industry, and the future of the Alliance.
In His Own Words
The Rowan Report:
We’re just about at the end of the first annual meeting since the merger of NHPCO and NAHC. What are your thoughts on how the event was received?
Dr. Steve Landers:
Yeah, it’s been great. You know, we have, we’ve had great attendance, and the energy has been good, and we’ve got diverse participation from people all throughout the care at home community from all over the country, and I think people learned a lot and got to spend time with friends and colleagues and do business. I’m feeling good about it.
RR: I assume you’ve learned alot and we’ll see some changes next year. Where will we be in 2026?
Steve: We’ll be in Washington, D.C. next fall. Also, our summer financial summit is still on the agenda. So, we’ll be in Boston and we’re hoping to see as many people out as possible.
Alliance Outlook 2026
RR: And your new board members, who start in January, were announced earlier. Sounds like you have some great people incoming next year. What is the focus for the organization in 2026?
Steve:
We are continuing to position ourselves as strong advocates in Washington for the issues that our members are facing. The whole board and team will be very much dug in and committed to putting the best possible effort forward on the big things that our members are facing from an advocacy standpoint. Of course, we want to continue to strengthen the member programming and the educational offerings. We are going to try to build on our partnership with the research institute for home care to try and add more research activities to the to the programming.
There are some things that we’re still not sure about how next year is going to look, because on the public policy front, we still have some kind of pending issues that we’re hoping get ironed out in a positive way. Depending on how the year wraps up, we could be very much still in a bit of a firefight, whether that’s the Medicare Home Health payment system, face to face certification access for hospice and home health services, or depending on if any type of Medicare Advantage legislation comes up. So there’s still a lot unknown about how the early year looks from an advocacy standpoint, but definitely, you know, with the existing board members and new board members and our team will be leading the way on those fronts.
Medicare Home Health Proposal
RR:
There are a lot of unknowns right now with the shutdown, the hospice carve out, and other issues we’re not really seeing any movement on. Is there any one unknown that is more challenging than others?
Steve: I think the most front and center issue is the Medicare Home Health payment proposal, because it was a terrible, misguided proposal that’s going to hurt lots of people, probably cost lives, cost the system more money, and so that’s definitely so visible and acute because it’s right with us.
If we see any more movement on this issue of hospice and Medicare Advantage that will certainly become more of an acute issue. We’re already taking it very seriously and are very actively and aggressively trying to push back that bad idea.
And, of course, the longer this government shutdown, the more harm there is with things like access to telehealth, so that’s high on our mind. There are a lot of other issues we’re concerned about with the future of Medicaid HCBS and the business environment for private duty home care as well. So, the list is long.
Advocacy
RR: Very long, indeed. During the opening keynote you mentioned a call for advocacy from everyone in attendance. Specifically, you mentioned presenting “one voice.” Are there current issues that has the industry divided?
Steve: I think we’re doing a good job of keeping people together. I think there’s always a risk when people get passionate and are wanting to solve problems. If we accidentally are publicly going in different directions, that’s not productive. I wouldn’t highlit any specifics, but I think, in general, the more we can come togehter on various issues because our goals are the same. None of us want to see care at home get cut back and over regulated. Everyone involved in these issues care about the same things. But, in Washington, when attention spans are very short, you only have so much political capital so we make sure we’re pushing for the same things in those advocacy efforts.
RR: Have you gotten any indication of where CMS is landing on the final payment rule? Last I heard, they had thousands of comments and feedback on the major cut.
Final Rule

Steve: They have received an incredible amount of comments. here have been meetings at all levels of the administration on these issues. We have outlined all of the aspects of this, from the access challenges to how cutting back home health is only going to lead to lead to higher overall expenses. We’ve given them a clear outline of the methodological flaws that they made in doing their calculations and their budget neutrality calculations. We’ve been very clear as well on where they have likely baked in data from pockets of fraud that are creating disadvantages for legitimate care providers in the way that the rate system comes out, So they have everything that they should need to reset these payments to where they should be based on the law. But, it’s a scary moment because they made this proposal in the first place, and at some point, somebody thought it was a good idea.
Keep Fighting
RR: What is the next step if the cuts happen?
Steve: If we don’t get what we’re hoping for, which is a real reset of these methodologies, then, the amount of teamwork and intense advocacy that’s going to have to happen to try to get Congress to fix this mistake is going to be enormous. And every one of us is going to have to put in whatever we can. Because, letting ourselves fall off of this type of cliff, letting patients and families fall off this kind of cliff, is just… it’s not… we’re gonna have to fight it every every step of the way. It’s just not right.
Commentary
The interview paused here. It was barely perceptible and nearly impossible to describe on paper. The depth of emotion conveyed in Dr. Landers’ words was palpable, sincere, and honest. In these few seconds, I was given the gift of insight on how completely Dr. Landers commits to this cause and how strong are his convictions. It was a powerful moment that I hope you all have the opportunity to witness.
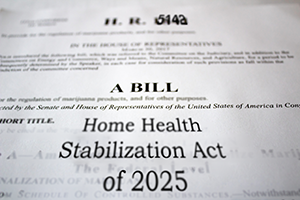
Home Health Stabilization Act
RR: Both you and your predecessor, Bill Dombi, have talked about how devastating these cuts will be. Estimates of 50% of home health agencies closing, reduced access to care, loss of jobs for caregivers, and especially devastating to the patients. What if this doesn’t change? Obviously, it’s going to take everybody working together. But what’s the first step? Is there a plan?
Steve: Oh, yeah, we’ve already been working with champions in Congress to introduce H.R. 5142 the Home Health Stabilization Act of 2025. If passed into law, would halt these cuts for 2026 and 2027 and allow time to work with Congress and the administration on more comprehensive, long term fix to this total mess that’s been developed by these flawed methods and give time to really work on comprehensive solutions to some of the fraud and abuse issues and potentially other reforms that could help. Now, anytime you’re trying to get an act of Congress passed, especially with a Congress that’s not open right now, with only so many days left in the legislative calendar, that’s no guarantee either, but that is the contingency that we’ve been developing.
If they don’t fix their proposal, they’re going to march forward on January 1 with another set of cuts that are going to lead to more delays in care and more people getting referred and not getting care and more rural and high poverty communities not haveing access to care and more people going back to the hospital and costing the system more. There are life and death issues. Not just an inconvenience or a cost. People can die. It’s a big deal.
RR: I think the industry as a whole feels like CMS is only looking at the financial numbers and not the consequences of what theyre doing. There are real people who are being damaged by these decisions.
Steve: Yeah, the proposed rule did not seem to take these things into account and it was not a patient- or family-centered proposal. It’s not a final rule yet. Their final action is pending and they need to address those issues. They have a responsibility, I believe, as public servants. I believe there’s a moral obligation here to revisit what was done and get it right.
RR: And, we do have some advocates at the congressional level, correct?
Steve: Yeah, we’ve been working with members of Congress to get them to weigh in with the administration, to tell them “get your final rule right.” We have been working on a contigency that if the rule is not done correctly that Congress would force them through legislation to stop the cuts. We’re not there yet, but we could be any day now. We’ve done that work with Congress to make that progress. That amount of advocacy will require teamwork. This is one of the reasons I was trying to emphaze the importance of unity if we end up with a very short calendar and a really hard problem to solve. It’s going to be pretty intense.
RR: And we’ll be right there with you if that happens, saying “how can we help?” I know this is the most pressing issue right now, but is there anything else industry-wise that you’re looking forward to and excited about?
Future Outlook
Steve: You know, I think it’s been fun and exciting and in some ways inspiring to see this alliance community grow and build. Whether it’s all these new and innovative AI solutions that our members are getting excited about, how they can improve workflows and efficiences, or whether it’s the attention for the storytelling around the issues that our members care about on social media and earned media. There are a lot of reasons to be excited and enthusiastic about the future.
I think the AI advancements have been really exciting and interesting for the industry, because there’s so much that can be done. And certainly, regardless of how big the cuts are, any cuts are going to be difficult for home health, and especially on top of what we’ve already had, yeah, but, you know, you being able to use these AI solutions to kind of cut some of the costs and things and offset that is, is at least a silver lining in some of it, and improve the worker experience, maybe in ways that make it a little less burdensome, and you can maybe keep more people in the
workforce.
RR: Well, I want to congratulate you. You’ve made it through your firstfull year in thisposition. I think there was a sense of this event being the test, the “How did the two organizations really come together and produce this huge thing,” and, it seems likethe blending of the home health with the hospice has worked really. Attendance is high and the vibe seems to be very positive.
Steve: You know, there’s a test every day. We have to keep trying to serve our community, and it’s a journey. We’ve got a great board, and a great team. They’re focused on the mission. The team came together nicely after the merger. Now that it’s settling down, we’re just going to keep working towards a bright future. Just keep at it.
RR: I think you’ve handled it all really well and the success of this event is a testament to that, as well as the other education and advocacy you’ve accomplished in the last year. I appreciate you taking the time to talk to me today. Keep fighting the good fight.
Steve: Absolutely. Thank you.
# # #


Kristin Rowan has been working at The Rowan Report since 2008. She is the owner and Editor-in-chief of The Rowan Report, the industry’s most trusted source for care at home news, and speaker on Artificial Intelligence and Lone Worker Safety and state and national conferences.
She also runs Girard Marketing Group, a multi-faceted boutique marketing firm specializing in content creation, social media management, and event marketing. Connect with Kristin directly kristin@girardmarketinggroup.com or www.girardmarketinggroup.com
©2025 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com








